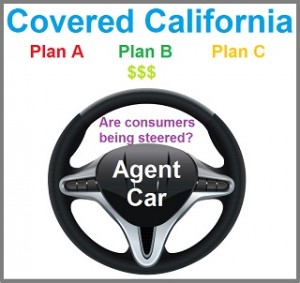
Are health agents steering consumers to the highest commission rate Covered California health plans?
Covered California has locked Certified Insurance Agents into representing all exchange plans to consumers and forbids agents from steering consumers to health plans with the best commission structures. Unfortunately, Covered California has no regulations that address any minimum compensation levels that the health plans or health insurance companies must pay agents for their efforts. Covered California announced over the summer that compensation for Medi-Cal enrollments would end for agents. Most recently Western Health Advantage (WHA) announced a split commission structure where Certified Agent enrolments would receive less compensation for Covered California plans than WHA’s off-exchange plans.
Different commission rates for each carrier
The reality is that each health plan or health insurance company has a different compensation or commission structure for agents selling their individual and family plans. Some of the carriers pay a flat one-time fee, others pay a fee per member per month, and yet others will pay a percentage of the total premium amount to the agent every month. In recent years agents have seen companies arbitrarily change commission structures in the middle of the year, develop a tiered commission structure to dissuade enrollments into high benefit Gold and Platinum plans, and split commission structures for on and off enrollments.
Western Health Advantage splits Covered California commissions
Western Health Advantage announced to agents on September 22nd that enrollments into their plans offered through Covered California will pay a flat $22 per member per month (pmpm). Individual and family health plans sold directly through WHA will receive a 5% commission. WHA did not give any reason for the change. The $22 pmpm can actually be a higher percentage of total premium amounts when the members are about 45 years old and younger for Silver plans. But the new flat rate quickly becomes less than the off-exchange 5% for consumers who are older and selecting higher premium Gold and Platinum plans.
Not all agents appointed with all carriers
While I don’t think most agents think too much about the commission levels when they are working with a consumer, there are definitely issues that will steer the agent in his or her plan presentation. First, if the agent works for a General Agency who isn’t appointed with all the carriers, that is a severe disincentive to even mention a health plan they don’t represent. Why would an agent help enroll a consumer for which they will receive no compensation because they are not appointed by the carrier to represent the plans and receive a commission? Even many independent agents like me are not appointed with all the carriers because of the paperwork and costs to become appointed. If a licensed health insurance agent has passed the tests to become a Certified Insurance Agent for Covered California, he or she should automatically be appointed with all health plans sold through Covered California. This would remove one hurdle from fairly representing all plans. An agent not appointed doesn’t necessarily have access to import plan documents such as the Evidence of Coverage.
Health plan bonuses may entice steering
The second factor that can steer agents into favoring one health plan over another to a consumer are any carrier bonus programs. Yes, health plan enrollments are still considered sales from the carrier’s perspective. Several of the health insurance companies will run programs that reward agents with bonuses for 10, 20, or more enrollments in their health plans. The marketing and sales departments for the health plans hope to create competitive cultural within the agent community where the top sales leaders are rewarded. Regardless of what the Covered California agent contract states, some agents are driven more by money than anything else.
Medi-Cal compensation stopped
In a letter announcing that Certified Health Insurance agents will longer be compensated for Medi-Cal enrollments, Executive Director Peter Lee reminded agents that, “Under Covered California’s contracts with all agents, which have been incorporated into regulations, agents must facilitate the enrollment of interested consumers into Medi-Cal.” During the first open enrollment back in the fall of 2013 I saw agents turn away Medi-Cal eligible individuals and families. That is still happening today. The agent bias against Medi-Cal is sure to expand now that agents aren’t even receiving a token compensation amount.
2015 Agent renewal agreement
Agents agree to represent all plans fairly, regardless of compensation, as stated in their agreement with Covered California.
- Representations.
Agent shall represent the plans offered through the Exchange in accordance with the following:
- Fairly and accurately present to Consumers all available enrollment options and prices regardless of the Agent’s appointments with any health plan;
- Unless specifically requested by the Consumer not to, when quoting prices, Agent shall fairly describe and display the health plans that the Consumer is eligible for;
- Explain to all potential Consumers about the availability of APTCs and that APTCs are only available through the Exchange.
- Agent agrees not to steer Consumers towards or against any of the QHPs sold by the Exchange solely on the basis of payment schedules or other consideration made to agent; […]
Covered California propped up the Navigators
Even Covered California acknowledged that enrolling consumers was no easy task when their Navigators complained about not meeting contractual enrollment goals and not being paid. Covered California went back and amended the Navigator contracts so grant progress payments weren’t necessarily tied to meeting the enrollment goals stated in the original contracts. This resulted in most of the Navigators receiving half their grants while falling far short of their enrollment goals.
Agent compensation should be equal between carriers
There should be no mystery about agent compensation. If Covered California wants to ensure that agents don’t steer consumers to a higher commission plan they should work with the carriers to set uniform compensation levels like Medicare. The Center for Medicare and Medicaid Services (CMS) sets rules for how Medicare Advantage plans sponsors compensate agents for enrollments. Agents must tell Medicare beneficiaries at the time of enrollment that they will be compensated. CMS publishes a spreadsheet of the compensation levels by State, county, and plan type. https://www.cms.gov/Medicare/Health-Plans/ManagedCareMarketing/AgentBroker.html
Covered California can exert influence to level commission structures
Covered California is the management that is setting the rules for an agent’s involvement with Covered California. Agents are the labor in the production of enrollments and who have no representation when it comes to negotiating their compensation levels. Covered California has acknowledged the important role that agents play in enrolling over 40% of all consumers in their health plans and a sizable percentage of Californians in Medi-Cal. If Covered California can work with the health plans to design standard benefit plans and negotiate plan rates, they can certainly exert some influence to make sure that equivalent agent compensation levels are established among all the carriers offering their plans.