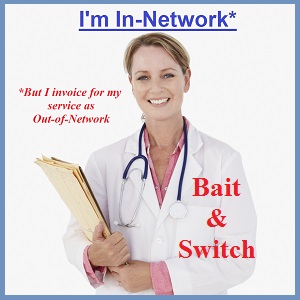
Some doctors are in-network for a health plan, but then invoice their services as out-of-network.
The narrow doctor networks of California’s individual and family health insurance plans are actually smaller than first thought as doctors use a bait and switch tactic to lure in patients and then bill for their services with “out-of-network” providers. The health insurance companies have little control over this practice that has a doctor listed as in-network for their health plan, but the services are actually billed by a facility that is out-of-network. This bait and switch tactic, aided and abetted by confusing online provider search tools and opaque billing statements and codes, leaves consumers paying more for health care services than they should.
Doctors in-network bait, switch to out-of-network billing
The great frustration for California consumers enrolled in individual and family plans, either through Covered California or directly with the insurance company, are the limited number of doctors in the carrier’s networks. While the carrier’s online search tool may show hundreds or thousands of physicians close to the consumer’s location, all those doctors may not really accept the Covered California health insurance. The office’s of some doctors will just tell potential patients that they don’t accept Covered California plans or only certain metal tier levels, even when they are listed as an in-network provider on the carrier’s website.
Covered California provider discrimination
But if the doctor blatantly practices discrimination against Covered California consumers, at least the families aren’t stuck with an over-priced medical bill because they are sent someplace else to receive health care services. Unfortunately, some Californians who thought they were visiting an in-network physician are being billed for out-of-network services. Instead of the billing being sent through with the physician’s tax ID number, who is listed as in-network with the health plan, the billing is done through the facility or medical group who is out-of-network. The result is that the consumer must pay several times more for the medical services because the provider is considered out-of-network.
Billing under medical group tax ID number
I had received several calls from clients who thought they were using an in-network PPO provider only to be billed for out-of-network services. In one particular instance I was able to contact the Anthem Blue Cross to see what exactly was happening. Anthem Blue Cross confirmed that the doctor my client had seen was indeed listed as in-network for their individual and family plan Pathway X network in California. Anthem Blue Cross also confirmed that the bill for the health care services came from the facility or medical group the doctor was practicing with. The health care services were billed under the medical group’s tax ID number. The medical group is not an in-network provider. The doctor attracted, or baited, the patient because of their in-network status with the health plan, but switched to out-of-network billing to increase their revenue.
Consumers can beg to be billed under in-network doctor
All Anthem Blue Cross could suggest was having the consumer go back to the facility and request that the services be invoiced under the physician’s tax ID number. Blue Cross mentioned that there may be good reasons why the services were billed under the facility such as the doctor had his own office (in-network) but also worked at the facility in question which was out-of-network. This particular doctor does work at the medical groups other locations. He is also a partner of the medical group according to their website. So even if the specific doctor is in-network with Anthem Blue Cross, but the medical group does all the billing under their tax ID number, the Anthem Blue Cross member receives virtually none of the benefits of their health plan.
Allowable Amounts for out-of-network
In this particular case, because the health care services were billed as out-of-network, the consumer had to pay the Allowable Amount set by Anthem Blue Cross for the services plus the invoiced amount above the Allowed Amount. Only the Allowed Amount accumulates toward the Anthem Blue Cross member’s out-of-network deductible. The excess amount is cash that is essentially thrown into the wind.
Only Allowable Amounts accumulates for the health plan member
The Allowed Amount is the cost of the treatment or service that Anthem Blue Cross and other carriers will recognize as the usual and customary rate (UCR) for out-of-network member services. For example, if a health plan member decided to use an out-of-network doctor to perform arthroscopic knee surgery the insurance plan has an Allowed Amount for the procedure, let’s say $1,000. The out-of-network doctor bills $1,500 for the surgery. If the member had not met their out-of-network deductible, only the Allowed Amount, $1,000, would be applied to the member’s out-of-network expense column. The insurance company doesn’t recognize the excess $500 over the Allowed Amount.
Doctor gets extra money with out-of-network billing
If the doctor was in-network, and actually billed for the surgery as an in-network provider, the health plan member would only be responsible for the contracted or negotiated rate, which might be just the $1,000. But if the doctor, who is listed as in-network, gets to bill for the Allowed Amount plus the excess amount, the physician gets their full retail price and the consumer gets screwed. One way to attract consumers into the out-of-network trap is to bait them with physicians who are listed as in-network, but have the out-of-network medical group bill for the services.
Independent medical groups have most confusion
This bait and switch tactic only seems to be happening at smaller independent medical groups. Larger physician groups associated with universities and hospitals don’t seem to be employing the revenue boosting out-of-network system. (Although, there are situations where medical group is in-network, but the hospital or facility where the procedure is performed is out-of-network.) Perhaps this is all a honest mistake on the part of these in-network physicians associated with out-of-network medical groups. I know that Anthem Blue Cross has worked with members to apply in-network copayments and coinsurance to some of the questionable out-of-network claims on a one-time basis for the members.
Health consumers must be diligent to find network status
It is unfortunate that consumers will have to take additional precautions to protect themselves from these bait and switch tactics. It is not enough to verify that the doctor is in-network with the health plan, the consumer must also ask, “Who will actually invoice me for the diagnosis and treatment?” Additionally, the consumer must inquiry if the billing party, if it is not the doctor, is in or out-of-network for their health plan. Only by rigorously questioning the doctor and medical groups billing practices can consumers really know if they are getting the benefits of the health plan they are paying for.