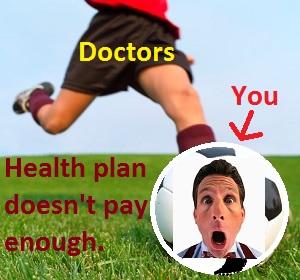
California doctors, upon finding that the new Covered California health plans may not reimburse them enough to maintain their vaunted lifestyle, are kicking existing patients with the new health insurance out of their practices. These doctors are the epitome of the maxim “Putting profits before people.” Most of these greedy doctors haven’t exercised the common decency to notify their current patients before their appointments that unless they have the right color of health insurance, they won’t be served.
Doctors kick out patients for profits
There has been significant confusion over which doctors and other providers are “in-network” with the various new individual and family plans offered in California. The main drivers for doctors suddenly pulling out of networks and kicking patients out of their practice center on the health plans automatic inclusion of certain providers and the physician groups poor communication habits. When doctors finally sit down and consider the new reimbursement rates they decide that loyal patients will just have to be sacrificed. After all, just because a patient has been with a doctor for over a decade means nothing when money is more important than people.
Doctors pull out of networks with no notice to patients
Numerous clients of mine have found out the hard way that their doctors are refusing to serve them at the health care counter. A few learned by researching which doctors were in-networks, others learned by having their new health plan rejected upon making an appointed or when they arrived at the doctor’s office. Even when we confirmed through the health plan’s provider search function that the doctor was in-network, their affiliated physician group pulled out of the network without notifying the existing patients.
Update June 29, 2014
The L.A. Times ran this story further illustrating how narrow networks are catching people off guard and causing additional expenses. While the article places much of the blame at the feet of the health plans, doctors also shoulder part of the responsibility by not being more involved in the contractual process.
Confusion over doctor lists is costly for Obamacare enrollees in state
Discouraging health insurance use
Some clients have reported to me that the admitting clerks of their doctor’s office have encouraged them to pay for the office visit out-of-pocket rather than use their health insurance. The rational is that by not utilizing the copayment of the health plan, and thereby paying the higher retail office visit price, the client would potentially save money if the office visit is denied by the insurance company. One would hope that the patient would be informed well in advance of the office visit if the care wasn’t to be covered. With most plans, the copayments add to the maximum annual out-of-pocket expense. Circumventing the health plan’s copayment system ultimately hurts the patient by making him or her shoulder a greater cost of health care services than the maximum limit of $6,350 for plans in California.
OBGYN boots mom out
Anthem Blue Cross EPO cards look like PPO cards
On March 25th I received a frantic call from a client because the doctor’s office just called and said they don’t accept the Anthem Blue Cross EPO plan she has been using to see her OBGYN. This expectant mother was told that the doctor’s office just realized she had a EPO (Exclusive Provider Organization) plan and not a PPO (Preferred Provider Organization) plan. PPO is printed right on the card. Also printed on the card is Pathway X Tiered which indicates an EPO plan, for insiders from Anthem Blue Cross. The Obstetrician-Gynecologist told the first time expectant mother that if she wanted to continue to see the doctor she would have to pay cash for her office visits.
CMA: doctors demand Anthem reimburse their claims
Doctors are demanding that Anthem Blue Cross reimburse them for services rendered before they realized the patient was in an EPO and the doctor wasn’t in the network. See – Anthem Blue Cross punishing patients and providers for their own error. Frankly, the doctors should have known the difference in the health cards and the restrictions of the EPOs. This is a perfect opportunity for the California Medical Association to fill the vacuum of information and help both doctors and patients sort through the new networks.
Doctors aren’t loyal to patients
I am fully aware that our preferred economic system is capitalism which lets doctors set their prices and choose their patients. It wouldn’t be unreasonable to politely inform prospective patients that the physicians group only takes certain health plans. But slamming the bus door in the face of a frequent rider is unacceptable behavior. Heck, there are laws mandating that health plans must offer refill prescriptions and continuity of care protocols when a member changes health plans. The very least these greedy doctors can do is see the patient one last time and renew any outstanding prescriptions.
Medical education subsidized by patients
Virtually every doctor has benefited from attending a public school funded with government money or a university that was subsidized by tax dollars. Many doctors interned at public hospitals that are supported by tax dollars and by Medicaid and Medicare reimbursements. If a doctor accepts Medicare Assignment, those office visit reimbursements are subsidized by federal tax dollars. In short, U.S. doctors have had their education and practices subsidized by tax payers. When we now have program to extend affordable health insurance to all Americans, some doctors are indignant that they would have to receive a lower reimbursement from the new health plans. How soon they forget who wiped their bottom when they were growing up.
Someone is lying about reimbursements
I can understand not accepting new patients because of the new health plan terms, but to deny services to existing clients just because the reimbursements are lower is just being greedy. Some offices inform patients they will only accept “off-exchange” plans as opposed to those sold through and subsidized by Covered California. Their explanation is that the identical off-exchange plan offers higher reimbursement levels for services. The carriers I have spoken with all claim that the networks and the reimbursement levels are the same for on and off exchange plans. So, someone is lying and I’d like to know who.
Secrets among thieves
Physician groups have every right to renegotiate higher rates. Perhaps they should unionize and go on strike refusing not to see any health plan members until the reimbursements rise. All of the problems are occurring with PPO and EPO plans. But the HMOs are equally responsible for not voicing opposition to the practice and being more transparent about reimbursement rates. I’ve also heard that the insurers include a non-disclosure clause in the contracts with doctors in order to prevent reimbursement rates from getting out to the public and their competition.
Hollow promise to protect patients
The California Medical Association, a group that represents patients proudly touts one of their top advocacy issues of protecting the physician-patient relationship.
Physicians view the doctor-patient relationship as sacrosanct, the very foundation of health care. This relationship stems from a physician’s primary ethical obligation – to place a patient’s welfare above their own self-interest and above obligations to other groups, and to advocate for their patient’s welfare. CMA passionately fights to protect this precious doctrine on multiple fronts.
CMA fiercely defends California’s bar on the corporate practice of medicine, which prevents corporate interests from unduly influencing physicians’ professional judgments in the name of profit and to the detriment of patients. Hospitals and other corporate interests do not have the same ethical and moral obligation to the patient as a physician does; therefore, it is essential to maintain the firewall between medical decisions and the corporate bottom line.
Inaccurate information and faulty rating programs can undermine the doctor-patient relationship. CMA has challenged Blue Shield’s Blue Ribbon recognition program that aims to identify doctors who meet certain care standards, but the data the health plan uses has inherent flaws and ratings are inaccurate and unreliable. CMA has worked with physicians to correct misinformation and asked Blue Shield to address the program’s fundamental shortcomings.
CMA also leads efforts in multiple arenas to leave the determination of what is medically necessary treatment where it belongs – in the hands of doctors. Health insurance gatekeepers and finance officers continually find new ways to delay and deny care, and erect barriers to medically necessary care for patients. Doctors are often a patient’s only ally in this David vs. Goliath battle that frequently entails mountains of paperwork and endless phone calls. Doctors believe it is a fundamental element of the physician-patient relationship to fight for their patients’ needed care to be delivered in a timely manner.
The recent actions by many California doctors seems to underscore that the CMA’s allegiance to protecting the physician-patient relationship ends when money is involved. Doctors have now become the “Goliath” that their patients must now fight with.
Doctors always win, patients lose
I doubt that anything will change because lobbyists and Super PACs that represent the medical profession pour too much money into the legislator’s campaign coffers. In California we are one of five states that prohibits hospitals from employing doctors. This law illustrates how the physician groups have been able to protect their members and achieve higher levels of income. As usual, a law that was meant to help families receive quality health care has been twisted to maximize the revenue of those who place profits before people.