CalHEERS Release Notes – 16.2
The California Healthcare Enrollment, Eligibility and Retention System (CalHEERS), also known as the online application, will be updated to version 16.2 on March 7, 2016. These release notes are intended to inform you of important changes to the functionality of the application.
[wpfilebase tag=file id=1426 /]
16.2.1 Reporting Income
Consumers who report income changes in the middle of the month are prorated by the application.
• The prorated monthly amount is calculated using the following formula:
o Monthly Income Amount times the Number of Paid Days in month (based on Beginning and End Dates) divided by the Number of Total Days in the month
• Certified Enrollers should discontinue the protocol of using multiple income entries to reflect mid-month income changes
Frankly, as an agent, I never did multiple income change entries. The small amount of APTC that is involved doesn’t justify the expense and potential errors within the CalHEERS program. If at all possible, instead of reporting a change to income, I adjust the APTC applied percentage on the Summary page if the income is increasing.
• Prior to 16.2 Release
o Example: Consumer received a raise on June 15
To report a mid-month income change accurately, two separate entries spanning the entire month in which the change occurred were entered separately
16.2 Release
o Example: Consumer received a raise on June 15
o Mid-month income changes will be automatically calculated and will not require separate entries
o Start and end dates of the income source will be used to determine the partial monthly income amount reported
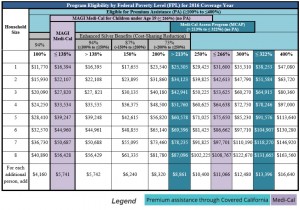
16.2.2 New 2016 Federal Poverty Level Guidelines for Medi-Cal Determinations
2016 Federal Poverty Level (FPL) guidelines are introduced to Medi-Cal eligibility determinations with the 16.2 release.
• CalHEERS uses the FPL guidelines to determine eligibility for Insurance Affordability programs such as Medi-Cal, Applied Tax Credits (APTC) and Cost Sharing Reductions (CSR)
• 2016 FPL guidelines are updated for Medi-Cal determinations only
o New consumers will first be evaluated for Medi-Cal eligibility, using the new 2016 FPL. If they are not eligible for Medi-Cal, they will be evaluated for Covered California (APTC/CSR) using 2015 FPLs, per regulatory requirements
Translation: For new enrollments under a Special Enrollment Period the new 2016 FPL will apply for Medi-Cal eligibility. If the household income is higher than the 138% of the 2016 FPL, then the CalHEERS program will evaluate the application under the 2015 income table ranges.
• Covered California consumers previously given APTC/CSR eligibility who report changes, will be reevaluated for eligibility and may find that they now qualify for Medi-Cal.
[wpfilebase tag=file id=1424 /]
• View the income guidelines with adjusted 2016 FPLs for Medi-Cal determination
[wpfilebase tag=file id=1425 /]
16.2.3 Former Foster Youth
The online application features updated fields and required information for consumers that attest to being Former Foster Youth (FFY). FFY who were in foster care on their 18th birthday or later, currently live in California, and are younger than age 26 qualify for free health care.
• FFY applicants will no longer be required to report Health Care, Tax, or Income information in the application
• FFY applicants have functionality to upload documents for verification of FFY status
o FFY applications will require administrative verification by a County Eligibility Worker
• For the question “Who is the Primary Caretaker of this child?” Foster Parent is an option
16.2.4 County Children’s Health Initiative Program
County Children’s Health Initiative Program (CCHIP) is a health insurance program that offers affordable and comprehensive medical, dental, and vision insurance for uninsured children age 0-19 who qualify. CCHIP is only available in three counties: San Mateo, San Francisco, and Santa Clara. See also: Medi-Cal prepares to snatch Bay Area children from parents.
For release 16.2, the online application will feature updated eligibility guidelines for CCHIP
• During the week of February 15, DHCS sent a notice to Covered California consumers who are deemed eligible for the CCHIP
• View our CCHIP Quick Guide for more information
[wpfilebase tag=browser id=241 /]
16.2.5 Preferred Method of Communication – Email Notice Implementation
Consumers have the option to choose either postal mail or Email as their preferred method of communication.
• For consumers with Email selected as their preferred method of communication:
o “Confirmation of Email Preference” notice is sent via standard mail to notify the consumer about their decision and that they will no longer receive paper mailings from CalHEERS
o For all subsequent new messages, consumers receive an email to alert them a notice is available for viewing in their Covered California Secure Mailbox
o Notice sent in English and Spanish with instructions in other languages to contact Covered California if assistance is needed
o Email notification is only applicable to CalHEERS notices
• When an invalid Email address reply is received, the Preferred Method of Communication is automatically updated to “Mail”
o A paper notice is sent to the consumer to inform them that an electronic notification was returned due to an invalid Email address
o The paper notice includes steps the consumer should take to change their Preferred Method of Communication back to “Email”
2016 Income Table, Covered California