A pregnant Bay Area woman who applied for health insurance through Covered California in November and has yet to receive any notification from her selected health plan or Covered California must now consider cancelling her prenatal doctor visits for lack of insurance. When asked about the status of the woman’s application a Covered California call center staffer said that it can take weeks for the insurance companies to receive the application. Essentially, Covered California has decided to ignore the woman, her family and unborn baby.
Original enrollment was early
When Mrs. L contacted me in mid-December she was already very concerned about the status of the health plan she purchased through Covered California and her impending doctor appointments in 2014. I could clearly see on my Covered California agent dashboard that Mrs. L had properly submitted an online application and selected a health plan for her family. Blue Shield, her chosen carrier, confirmed to me that they had no record of Mrs. L’s application from Covered California.With fading hope that Covered California would actually transfer the data to the carrier, we initiated another application.
Covered California fails to transfer data a second time
When I called Blue Shield on December 31st they still had no record of Mrs. L’s application. After repeated attempts, hours on hold and dropped calls, I was finally able to speak to a Covered California call center staff member. She confirmed that Mrs. L did have two applications in the system; the first one Mrs. L initiated in November and the second I created in late December. She withdrew the first application but had no explanation as to why it neither application had been forwarded to Blue Shield.
Covered California blames carriers and agents
Covered California told me in the early months it was taking several weeks for the application data to actually reach the carriers and be uploaded to their system. They also insinuated that agents submitting second applications might also be the cause for the problems. However, I have had clients who received two invoices from the same carrier for the same amounts because two application were successfully transferred by Covered California to the health plan.
The doctor appointment is on Monday, January 6th
Regardless, Mrs. L had a doctor appointment for her pregnancy on January 6th and I asked the Covered California staffer what I was suppose to tell my client since Blue Shield had no record of her application, she has no invoice, no member ID number, her name isn’t matched on the Blue Shield binder payment website, and she applied over 6 weeks ago? The sound of silence I heard was of Covered California ignoring a pregnant California resident for whom they promised to helped.
January 9th update: Blue Shield still has no record of Mrs. L’s family in their system. Covered California insists it is not their problem and many applicants are experiencing the same problem. The original application of Mrs. L was mysterious “re-activated” at Covered California with a 2/1/2014 effective date.
The Covered California black hole defies explanation
I wish I could say this was an aberration but it isn’t. I have several clients who applied for coverage months ago and still don’t show up in the system of any of the health insurance companies. It doesn’t seem to make a difference if it was a paper application, client created account and application or if I, as a Certified Agent, generated the application, some enrollments at Covered California just drop into a black hole.
Disappearing applications at Covered California
The Covered California system even dropped one of my applications from my client list. This gentleman, who is mentally handicapped, had a paper application sent in on his behalf in November. When his guardian had heard nothing from Covered California she contacted me. Covered California had no record of his application so I created one for him online. A couple days later when his guardian sent me proof of residency for me to upload to his account, the gentleman’s’ application was gone.
No accountability
Covered California had no explanation as to why the application was dropped. This man needs to see his physicians on a regular basis. Covered California has jeopardized his health that of Mrs. L’s and scores of other people by a poorly designed and/or operated system. If Covered California would have been a Medicare Advantage contractor the Centers for Medicare and Medicaid would have put them on sanction weeks ago and probably issued a civil monetary penalty also. Covered California, like so many bureaucracies, are accountable to no one that really matters like the consumer. See CMS sanctions CVS SilverScripts Part D Prescription Drug Plans
California elected officials ignore exchange failures
The state of the situation is that no one in questioning the operation of Covered California. No one in elected legislative or executive office or the media is inquiring as to why Covered California is failing the residents they were created to serve. One of the mission statements of Covered California is
The Exchange will be a catalyst for change in California’s health care system, using its market role to stimulate new strategies for providing high-quality, affordable health care, promoting prevention and wellness, and reducing health disparities. – California’s Health Benefit Exchange
Their current actions are actually increasing health disparities and hurting the health of Californians.
Who designed the data transfer system?
One client was able to pull out some information from a health insurance carrier as to why it was taking so long from “application to invoice” through Covered California. He reported the conversation to me in an email.
Basically, what she told me is that they’re dealing with several unrelated computer systems – when they receive that data from Covered California, it has to be manually entered into their “application” system, then it gets printed out and sent to the “enrollment” department, where it is manually entered again (this is where their bottle neck seems to be). After the “enrollment” phase is complete, then the payment processing department does their job. None of their computer systems seem to be linked, and certainly not with Covered California’s system.
It doesn’t help that Covered California is taking so long to verify and send the data over to the carriers. I checked on Mrs. L’s application and the date stamp for a Covered California employee that actually submitted enrollment to Blue Shield was January 3rd.
Covered California hurricane destruction
Covered California created their own hurricane level destruction by refusing to extend health plan cancellations to March 31, which created a crush of last minute applications, which in turn melted down the website on December 23rd. They then extended the deadline until December 28th because they knew their system had crashed as people were enrolling. Now they are in the impossible position of getting the enrollments sent to the carriers for billing by January 6th for retro-active effective dates of January 1st.
Just beg your doctor to keep the appointment
Instead of apologizing for the chaos they have created, Covered California is asking people who have no health insurance in their hand to beg their doctors to keep their January appointments.
Can I go to my health care provider starting January 1st if I have not paid yet?
As long as you pay by January 6th, you can use services covered by your health plan starting January 1st. First, be sure the provider (a doctor or other health service provider) is participating in the health insurance plan network you have selected. The provider may ask you to sign a statement agreeing to pay for the services if you cannot eventually prove you have health insurance. The provider may later send you a bill (“claim”) for the care. Once you have proof of health insurance coverage effective January 1, 2014, which you will receive after you pay for the insurance, you can submit the claim to your health plan to pay. It is also likely that by the time you get a bill or claim from your provider, you will already be entered into your health plan’s system. Simply call your provider and have them re-submit their bill directly to your health plan. Call your health plan to ask if the provider is in their network, if you have questions about whether a service is covered (included in your insurance plan) or about how to use your coverage. See the chart below for Covered California health plan contact information. – Using Coverage Starting January 1, 2014
Covered California adds to confusion with congratulatory email
Covered California originally wanted to allow residents to make their first premium payment right through the Covered California web portal. There is even a dead link for making a payment on the application/account web page. Why they chose not to include the payment system on the site is anyone’s guess. To rub salt in the wound of people who have applied for health insurance and received absolutely nothing, Covered California finally figured out how to use their email system and sent scores of accounts a reminder to pay an invoice that most of the people have never received. Can you say irony?
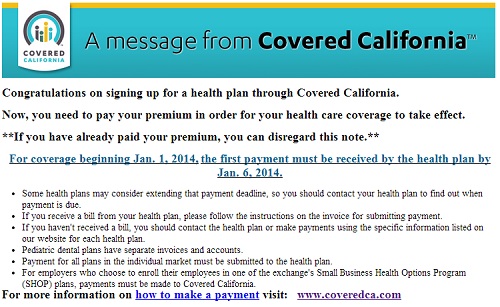
Ironic message from Covered California for those who have not received an invoice.
They followed the rules and got ignored
Perhaps the most frustrating aspect of the Covered California debacle is that it is happening to people who have steadfastly maintained their health insurance, followed the rules posted by Covered California and have been scrupulously honest on their applications. Many of these people are now facing the prospect of no health insurance in January 2014 because of the very institution that promised to make health insurance easier, better, faster and cheaper. Covered California shouldn’t make promises they can’t keep.