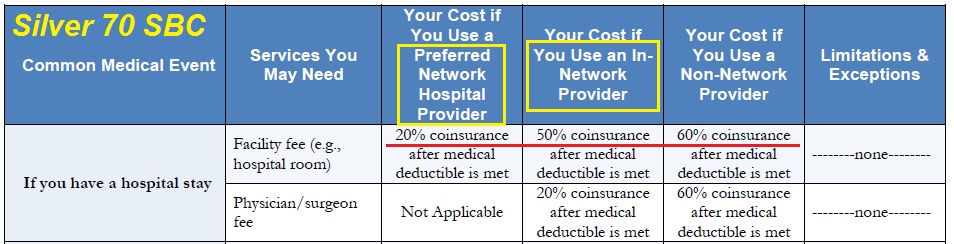
Tier 2 hospitals in Blue Cross’ Tiered PPO networks can have cost sharing coinsurance percentages double that of a Preferred Tier 1 hospital.
In 2016 Anthem Blue Cross introduced their new Tiered PPO Network health plans in four counties of California. The Tiered PPO marketing literature noted the member’s cost share would be less if he or she used a Tier 1 hospital, but it didn’t indicate how much less expensive it would be. There can be some confusion when referencing the official Summary of Benefits and Coverage for the Tiered PPO plans because it never uses the terms Tier 1 or Tier 2.
Higher Tiered PPO coinsurance
Blue Cross introduced the Tiered PPO plans in the California counties in 2016 that had previously offered EPOs (Exclusive Provider Organizations): Los Angeles, Orange, San Diego, and San Francisco. If you live in one of these counties you can only purchase a Tiered PPO plan from Blue Cross regardless of whether you enroll through Covered California or go directly to Anthem Blue Cross. EPO plans have no out-of-network coverage similar to an HMO. The Tiered PPO allows the members to go to hospitals that may have been out of network under the EPO plans, but they’ll get socked a hefty Tier 2 coinsurance percentage.
Preferred Hospital Network Provider Tier 1
Blue Cross put out a list of Tier 1 and Tier 2 hospitals for the affected counties, and discussed the higher member cost sharing, but there were no numbers attached to the document. (Review tiered hospital list at end of post.) The actual member cost’s for all health plans is contained in the federally mandated Summary of Benefits and Coverage (SBC) document. Whereas most PPO SBCs will list the cost sharing for in- and out-of-network providers, the Blue Cross Tiered PPO SBCs have another column called Preferred Hospital Network Provider. This Preferred Hospital Network Provider column is represents the cost sharing the member responsible for if they use a Tier 1 hospital. SBCs for Blue Cross 2016 plans can be found on my download file tree page.
In-Network Provider Tier 2 Hospitals
The Tier 2 hospital coinsurance cost sharing percentage is listed under the column In-Network Provider. Usually, the In-Network Provider column displays the lower coinsurance percentage relative to the Out-of-Network Provider column. The only providers that are tiered and have different cost sharing percentages under Blue Cross Tiered PPO plan are hospitals. There are no Preferred Physicians. Doctors are either in-network or they are out of network. And, all hospitals are Preferred Hospital Network Providers in case you need emergency room treatment.
Tier 1 & 2 Coinsurance percentages by health plan for 2016
| Anthem Blue Cross | Tier 1 | Tier 2 |
| Tiered PPO Health Plans | Preferred Hospital Network | In-Network Network |
| Bronze 60 H.S.A. | 40% | 50% |
| Bronze 60 | 100% | 100% |
| Bronze 5000/25% | 25% | 50% |
| Bronze 5750/20% | 20% | 40% |
| Bronze 6600/20% | 20% | 50% |
| Silver 70 | 20% | 50% |
| Silver 73 | 20% | 50% |
| Silver 87 | 15% | 30% |
| Silver 94 | 10% | 20% |
| Silver 1750/30% | 30% | 50% |
| Silver 2000/25% | 25% | 50% |
| Gold 80 | 20% | 50% |
| Platinum 90 | 10% | 40% |
Tiered coinsurance percentages are the same whether the plan is purchased on- or off-exchange.
The penalty for going to a Tier 2 In-Network hospital is a coinsurance percentage of over double for most Tier 1 Preferred hospitals. Although, the higher coinsurance still goes toward meeting your calendar year maximum out-of-pocket amount for the year. So if you know that you are going to hit the maximum out-of-pocket (MOOP) amount with a combination of different health care services, utilizing a Tier 2 hospital with higher coinsurance is of little consequence. It just helps you hit the MOOP sooner. The significantly higher coinsurance percentages for using Tier 2 hospitals is Blue Cross’ attempt to steer members toward hospitals Blue Cross may have more favorable claims reimbursement contracts with.
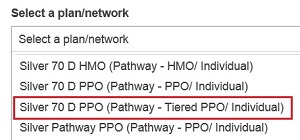
When performing a provide search on Anthem Blue Cross website, and you reside in L.A. Orange, San Diego or San Francisco counties, always select the Pathway – Tiered if you have an individual and family PPO in one those counties.
Tiered hospitals may be a welcome design
While it may be a shock that your favorite hospital is Tier 2 and have hefty coinsurance attached to it, there are many people who would gladly accept triple the coinsurance percentage just to use certain hospitals. In Northern California, Blue Shield has completely removed all Stanford physicians and hospital from in-network status. Many people would gladly pay a higher coinsurance to see their Stanford physicians as in-network providers. (Coverage for out-of-network providers may be limited by additional deductibles and restrictive allowable amount reimbursements which can trigger high balance billing scenarios for plan members.)
Better than an EPO?
The health plans are gambling that most members will not meet their calendar year maximum out-of-pocket amount. If the plan member utilizes a Tier 2 hospital, the health insurance will have to shoulder less of the cost for the procedure. More of the risk for the hospital bill is transferred to the patient. The Tiered PPO Networks are an improvement over the more restrictive EPO plans. If the tiered hospital system works to hold health insurance premiums we may see more health plans move into the tiered provider heath plan design.
[gview file=”https://insuremekevin.com/download/anthem_blue_cross/ifp_2016/ABC%20Tiered%20PPO%20Hospital.pdf” height=”600px” width=”600px” save=”0″]
[wpfilebase tag=file id=834 /]