Anthem Blue Cross announced on October 9th that certain small group health insurance plans regulated by the California Department of Insurance will receive a one-time credit on their December invoices. Similar to the one-time credit of 18% issued by Blue Shield in September, there was no additional information about what prompted the credit beyond a review of past plan filings. If nothing else, it’s nice to know the California bureaucracy of the CDI is actually watching out for the consumer now and again.
Anthem Blue Cross announced on October 9th that certain small group health insurance plans regulated by the California Department of Insurance will receive a one-time credit on their December invoices. Similar to the one-time credit of 18% issued by Blue Shield in September, there was no additional information about what prompted the credit beyond a review of past plan filings. If nothing else, it’s nice to know the California bureaucracy of the CDI is actually watching out for the consumer now and again.
Text of press release below
Premium Credit for Anthem Small Group in December 2012 CDI-Regulated Medical Plan Business only
Your Anthem Blue Cross Life and Health Insurance Company (Anthem) Small Group clients will receive a one-time monthly medical premium credit of 8.21% on their December bill for members enrolled in plans filed with the California Department of Insurance (chart of plans below). The credit will be based on enrollment from the group’s September billing statement. We ask that you communicate this news with your clients. Anthem will email communications to employers the week of October 15th. This premium credit is a result of ongoing discussions and an agreement with the California Department of Insurance related to past medical plan filings. Because this premium credit is only applicable to select Small Group medical plan clients (those currently on plans regulated by the CDI), there are a few important points to be aware of:
- The credit will be based on enrollment in Anthem Blue Cross Life and Health Insurance Company’s CDI-regulated medical plans as of the group’s September 2012 billing statement.
- The credit will be based on the medical premium associated with enrollment for September 2012 as of September 30, 2012.
- Example – an employer with three covered employees on the Solutions 2500 PPO with combined monthly premium of $1540 would receive a credit of $127.00
- This credit will not apply to groups new to Anthem Blue Cross Life and Health Insurance Company small group effective in October, November or December, 2012
- The credit will appear on your client’s December billing statement. Clients must be an active Anthem Small Group in December to receive the credit.
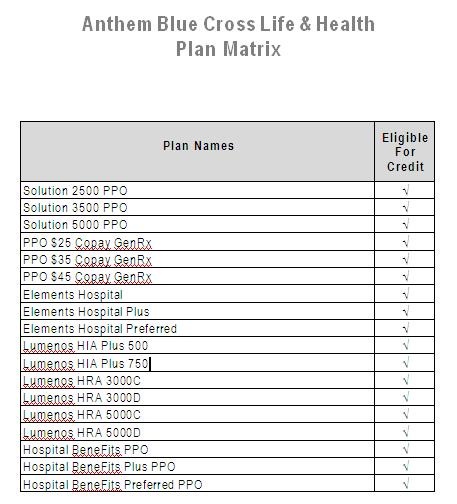
- A listing of Anthem’s Small Group CDI-regulated medical plans is included below.
- This premium credit will not impact agent commissions.
- The credit will not apply to Anthem’s 51-99 EmployeeElect customers.
- The credit will not apply to CalChoice members on Anthem products.
- The credit will not apply to Anthem Blue Cross small group products (plans regulated by the Department of Managed Health Care).
We will be sending e-mails to impacted employer groups in mid October to inform them of the premium credit.