If you believe that Covered California has erred in an eligibility determination regarding health insurance enrollment or subsidy, you can file an appeal. Appeals are a last resort to fixing a problem with your health insurance through Covered California.
Covered California Erases Your Subsidy For Health Insurance
Many of the intractable errors occurring with Covered California are all decisions that happen behind the scenes. The CalHEERS application software is grabbing information from other federal and state databases and applying it to your application for health insurance and the Advance Premium Tax Credit subsidies. This gathered information combined with data you put on your application can translate into results or eligibility determinations that are adverse to you.
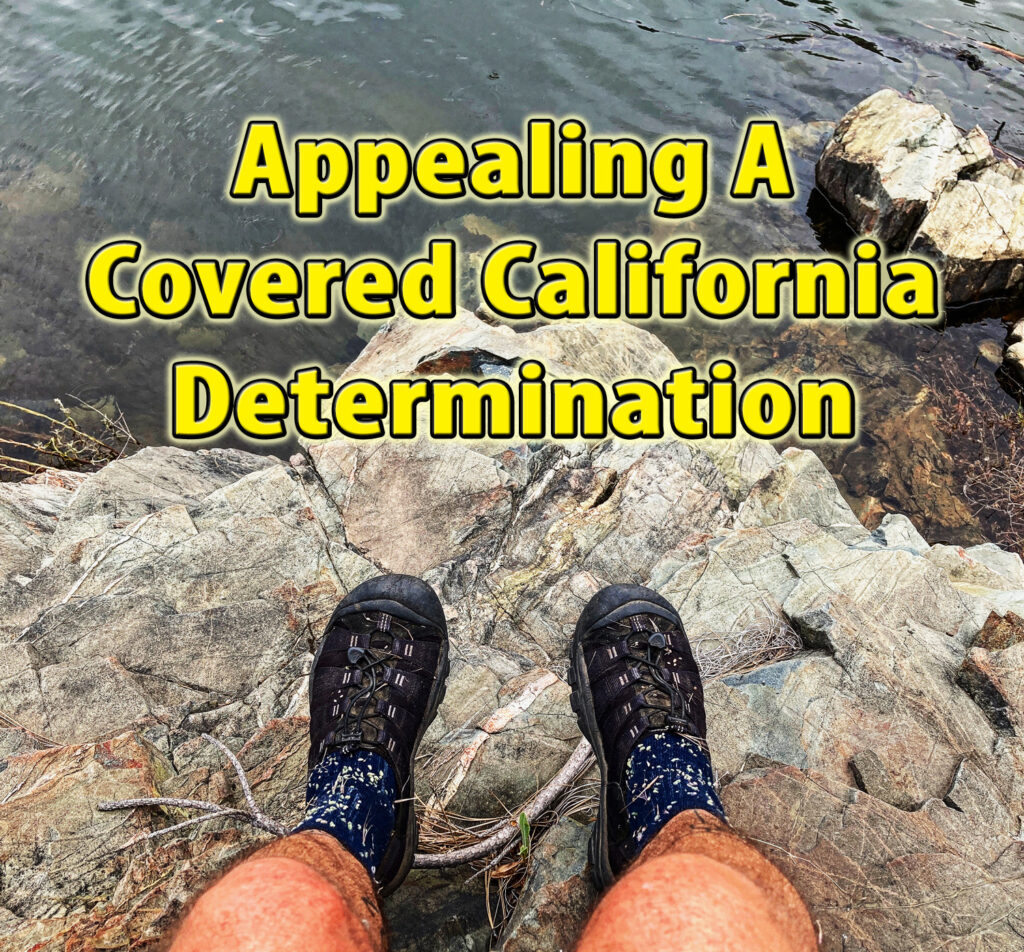
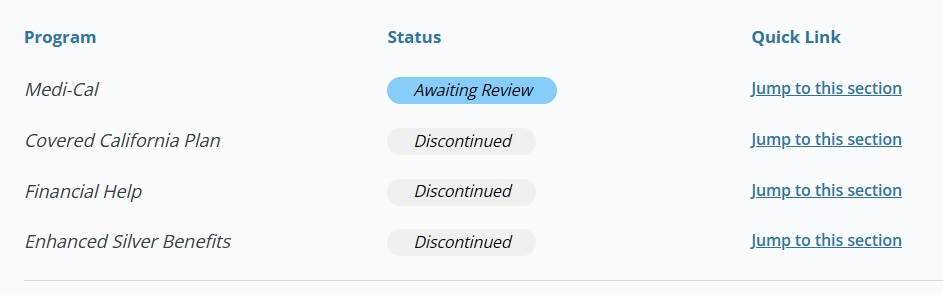
Common issues for 2024 are household members for whom no subsidy is being offered or the denial to the household member to even enroll in a health plan. Most of these problems were briefly mentioned in a letter Covered California generated at the time of renewal for the 2024 plan year. Unfortunately, many people did not carefully read the letter or never received it.
File Appeal as a Last Resort Relief
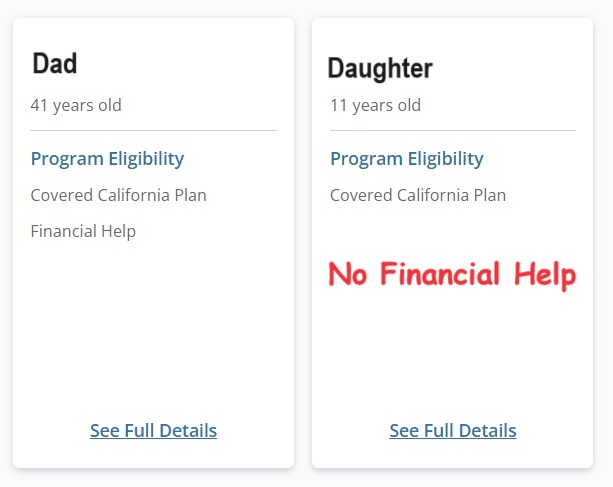
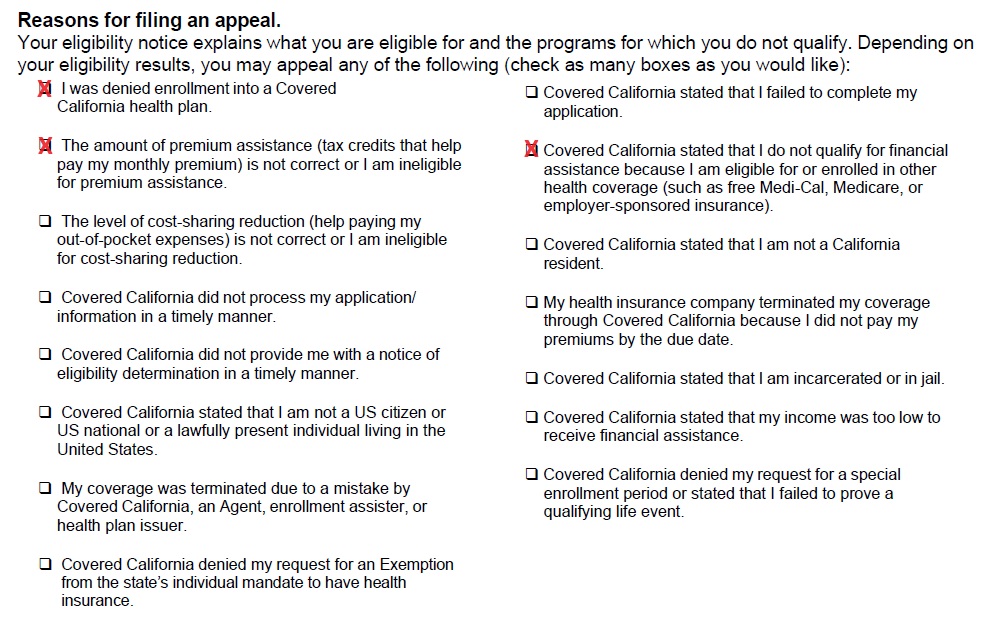
Compounding the consumer confusion is the lack of details related to why no subsidy is offered or the person cannot enroll in a health plan. The letter may only state, “Our records show that you are eligible for or enrolled in health insurance from your job (or a family member’s job) or a government program such as Medicare or Medi-Cal.” Covered California does not tell you where they got such information or what job or government program you may have.
It appears that most of the subsidy denials are for potential enrollment in Medi-Cal. Of course, your child may have received subsidies for the last couple of years with no issues. Now, suddenly, Covered California thinks you or the child has Medi-Cal. Who do you call? Covered California can give some information or clues, but it is incumbent upon the consumer (You, Mom, or Dad) to investigate it.
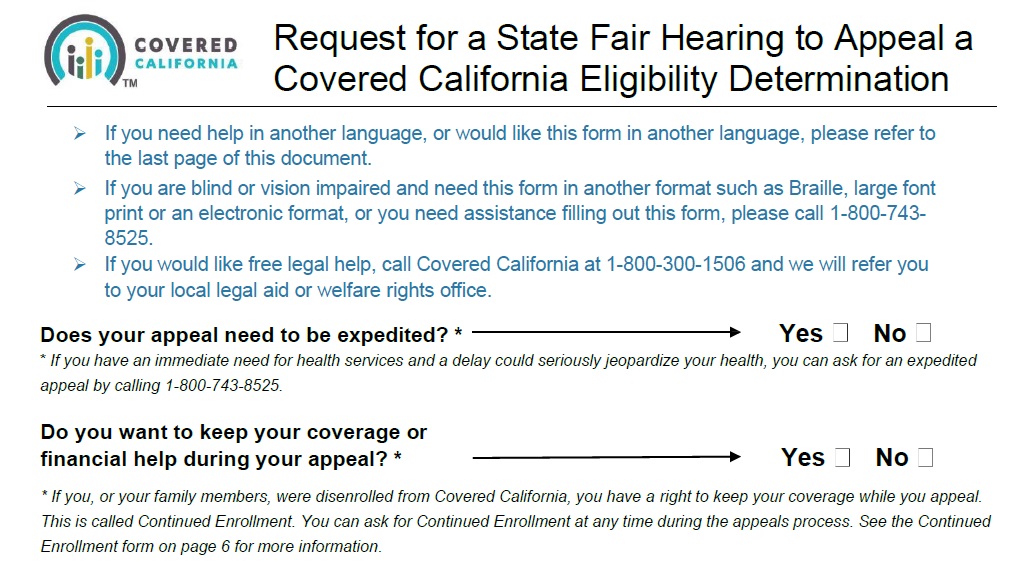
If you are totally stymied, you can file an appeal with Covered California. You can file online using a Doccusign application or download the appeal PDF. The document is titled “Request for a State Fair Hearing to Appeal a Covered California Eligibility Determination.” The hearing is before an administrative law judge. Covered California does not want to resolve most problems through the appeals process.
What the appeal does is escalate the issue where actual humans review your case. If you have no help or satisfaction from working with your agent or the Covered California customer service staff, an appeal may be your last resort. You may get detailed information that helps you track down the erroneous data that triggered the denial or loss of subsidy.
On the appeal paperwork you can indicate the nature of your appeal such as denial of enrollment or incorrect calculation of subsidy or financial assistance (APTC.) As an agent, I have had modest success escalating certain issues directly to the agent service center. This leads me to believe an appeal, where real people focus on the specifics of your case, can either correct the erroneous data or give you the information necessary to fix the problem.
Benefitscal.com Account May Help With Medi-Cal
What seems to be a new problem is the determination that some of the household members are offered or enrolled in Medi-Cal. This all seems to have occurred when the Covid Public Health Emergency ended and Medi-Cal resumed normal operation. Some counties, within their databases, are listing some people eligible for Medi-Cal. Covered California picks up on the Medi-Cal eligibility and denies any subsidy. You must contact the county that has the erroneous data and get them to correct it.

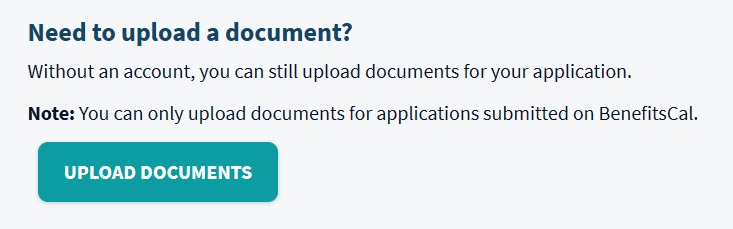
Some people have had success in communicating with the county Medi-Cal office using Benefitscal.com. Once you learn that Medi-Cal is precluding the subsidies, and you learn which county is the offending agency, you can create a benefitscal.com account to upload documents to review by a case eligibility worker.
Tips from people who have used benefitscal.com is that you still need to call or communicate with the county to inform them the documents are sitting in the benefitscal.com account. One of my clients was able to complete the process within a couple of weeks using benefitscal.com. The subsidies were restored for her son beginning the next month.
Unfortunately, consumers should not have to go through this byzantine process of becoming private detectives to learn why they were denied enrollment or the subsidies. Covered California should spell out the specific reason either in a letter or on the phone. However, when all else fails you can file an appeal to kick the human process in gear to review your account.