
New Covered California updates for 2017 will trigger letters to be sent employers of consumers about their health insurance enrollment through Covered California.
Covered California has given their online health insurance enrollment system a serious make over with the release of the CalHEERS 17.2 build. Not only has the user interface been enhanced, members must now enter their employer’s contact information before they will be eligible for the monthly subsidy. In addition, Covered California will begin notifying a member’s employer when they enroll or renew their Covered California health insurance.
New Employer Contact And Notification Letters
Covered California routinely updates their CalHEERS (California Health Insurance Eligiblity Enrollment and Retention System) to correct glitches and add other enhancements. The updates also include modifications for enhanced screening of individuals and families for eligibility for the Advance Premium Tax Credits (APTC) also known as the monthly subsidy.
The newest eligibility screening function is the mandatory reporting of a member’s employer contact information.
CalHEERS 17.2 Release Notes Employer Contact
Release Note: Employer Contact Information is now required for all online applications with APTC eligibility
Previously, the online application did not require users to complete the ‘Employer Contact Information’ section of the Personal Data – Health Insurance Information page of the application before enrolling in a plan for APTC eligible/conditionally eligible consumers.
Now, consumers with APTC conditional eligibility or eligibility are required to provide this information on the online application in a new section titled Employer Contact Information, accessible via the Actions pane on the consumer homepage or after viewing the Eligibility Results page.
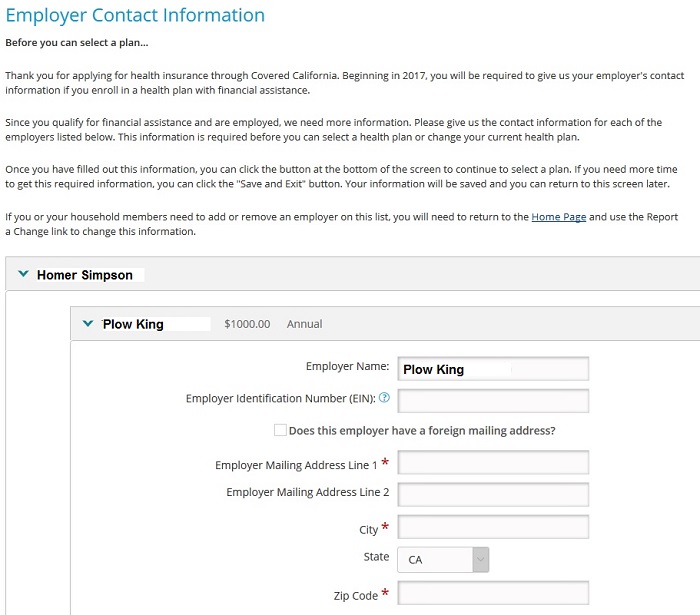
Covered California consumer must enter employer information before they can become eligible for the monthly tax credit subsidy.
Self-Employed
Covered California states that self-employed individuals should just enter their own name and address for the employer. Technically that is not correct, but is is the only work around solution Covered California has until they think of a better system to notate self-employment.
Covered California To Send Consumer’s Employer A Letter
But Covered California isn’t stopping with just getting the member’s employer address, they are going to use it. Covered California will begin sending out letters to the member’s employer (as if Covered California doesn’t already send out enough annoying letters).
CalHEERS 17.2 Release Notes Employer Notices
Release Note: Employer noticing will become automated to notify employers that their employees have coverage via the Exchange
Previously, when consumers provided Certified Enrollers with income information and optional employer contact information on the Healthcare page of the online application, there was no reconciliation or notification to employers regarding their employees enrolling in coverage via the California Health Exchange.
Now, Covered California will send notices to employers when their employees have a Covered California plan in the enrolled status and:
1) When a consumer has an Initial determination of eligibility for APTC with active employer income
2) When a consumer renews for the next benefit year, is eligible for APTC with active employer income
3) When a consumer, who is eligible for APTC, reports a new current employer
4) When a consumer, who is eligible for APTC, updates employer information and an employer notice has not been generated in the benefit year
A copy of the employer notice will automatically upload to the consumer’s Documents & Correspondence page for reference.
There are probably several reasons why Covered California feels it is necessary to divulge a family’s health insurance information to an employer. Under the Affordable Care Act, Applicable Large Employers (ALEs) face a tax penalty if any of their employees receive a tax credit subsidy from a Marketplace Exchange such as Covered California. It’s also possible that the employer offers affordable health insurance to the employee. The affordable health insurance offering makes the employee ineligible for the tax credit subsidy. Covered California may also want to develop their own database of employers that they can market their Covered California Small Business health insurance program to.
Income Section Make Over
Covered California has acknowledged that the Income Section of the application was confusing to most people. The three separate income types of Employment, Self-Employment, and Other Income, coupled with a Deduction sections spoke to bookkeepers and CPA, but not normal consumers.
CalHEERS 17.2 Release Notes Income Section
Release Note: Income Pages Enhancements
Previously, the online application contained income questions that created too much variance in the way income was entered. Depending on the end user, if was confusing and difficult to understand.
Now, there is a re-designed Income section of the Online CalHEERs Application that will change the way income is entered. The improvements include:
-
Income page language upgrade
-
Implemented income grouping with smart form technology
-
New hover text added
-
Added American Indian/Alaska Native (AI/AN) income subtype that is countable for Magi-Medical
-
Income is now counted for Registered Domestic Partners
-
Other Taxable Income replaces the ‘Miscellaneous’ option for the ‘What type of Income?’ Dropdown on the Add Other Income page
-
Lump sum income reported in the month of application triggers an additional eligibility run (month of application and for the month after application) when at least one member is not found MAGI M/C eligibility
Covered California adds easier navigation for 2017.
The new Income section looks more like an income tax preparation software. Instead of three income categories, the new income section will sport 22 categories. A more defined income category helps to match the consumer’s uploaded verification for the income reported. For example, if a consumer lists $500 per month of interest income, they can supply a 1099 that corresponds to the particular interest income category. Before the income enhancements, consumers entered interest income under the Other category and it may not have been as obviously to Covered California the uploaded verification documents corresponded to.
However, the enhanced income section still doesn’t address the issue of estimating income for self-employed individuals. The new income enhancements have not abandon the concept of trying to capture the exact amount of a household’s future Modified Adjusted Gross Income (MAGI). No tax payer knows what their final MAGI will be until they complete their tax return. If the new income section helps consumers avoid under reporting their income and then having to repay any excess APTC on their tax return, then the enhancements are a success. But the weak link is getting people to update their income when there is a job change or shift of self-employment income.
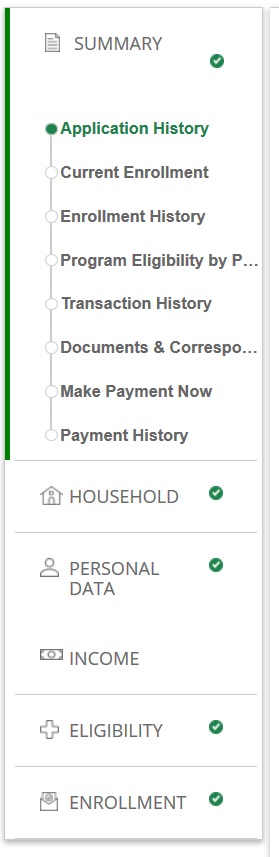
A major improvement is the addition of a left sidebar menu that mirrors the progress check boxes across the top of the application. This allows people to more easily navigate the application to review the household application data. By clicking on one of the page headings, the section is expanded in a drop down menu format to reveal the subsection. For instance, by clicking on Personal Data, the consumer or agent can quickly navigate to the Address, Demographic Data, Tax Information, Health Care, Optional Data, and Summary portion of the section.
Uploading Documents To Covered California
Another improvement will be allowing the consumer to upload documents even if there is not a request to verify an item such as income or residency. Covered California consumers have received letters requesting them to verify some aspect of their application. The Manage Verification link, which allows consumers to upload documents, was at times no longer active. Now people can upload new documents through the Documents and Correspondence page of the Summary section of the application.
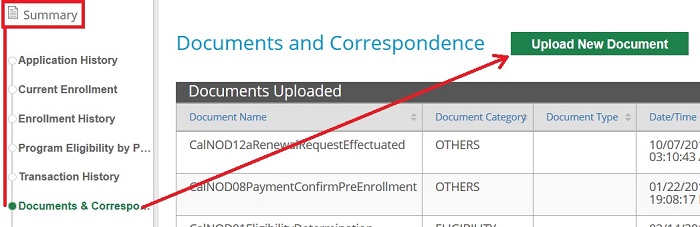
Covered California consumers can now upload documents through the Documents and Correspondence page of the Summary section.
CalHEERS 17.2 Release Notes Document Uploads
Release Note: Verification Documents can now be uploaded to the Documents & Correspondence page regardless of eligibility or case status
Previously, documents could only be uploaded on the Documents and Correspondence page if the case was in a Conditionally Eligible status only.
Now, documents can be uploaded on the Documents and Correspondence page regardless of eligibility or case status (even if case is terminated). There are also two new buttons on the Documents and Correspondence page: Upload New Document and Link to ECM Document. The ‘Link to ECM Document’ is used to link
Documents mailed or faxed in by the consumer to the Covered California back office. Certified enrollers should access the ‘Upload New Document’ link to attach documents to the consumer’s case.
Overall, the upgrade to the Covered California application will be beneficial for most consumers and agents working with the system. The new notification letters alerting employers about an employee’s health insurance through Covered California will likely be seen as an invasion of privacy on the part of some members and be met with confusion by employers. While I understand that Covered California is just trying to comply with the ACA rules concerning verifying eligibility for the APTC, there will be some people who feel they are crossing a line of privacy with the employer notifications.
CalHEERS 17.2 Release Notes
[wpfilebase tag=file id=2108 /]
Covered California 2017 Income Page Enhancements
[wpfilebase tag=file id=2109 /]


