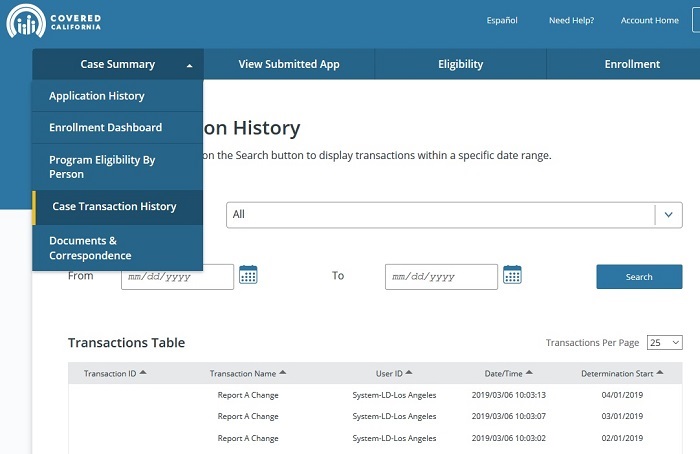
Covered California has modified the look and feel of their CalHEERS online application and enrollment portal beginning in May, 2019. The pages and flow for consumer plan selection and cancellation have been revised and should be slightly easier for consumers to navigate. Lost are access to the eligibility by person Medi-Cal aid codes and the documents and correspondence section.
Enrollment Dashboard
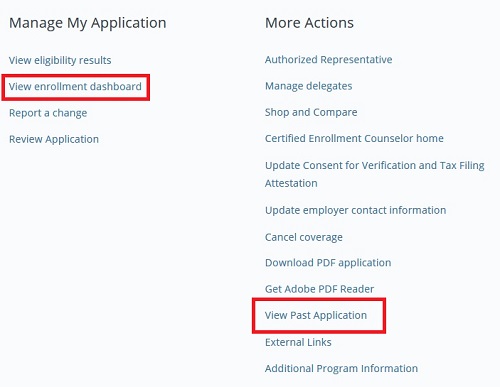
With the CalHEERS release 19.4, Covered California completely wipes away any vestiges of the original online account and application launched in 2014. The new updates to the plan eligibility, enrollment, payment, and cancellation is now under the new enrollment dashboard. While this should be more intuitive consumers who manage their own accounts once a year, the new 19.4 release hides information that can help the consumer and agents.
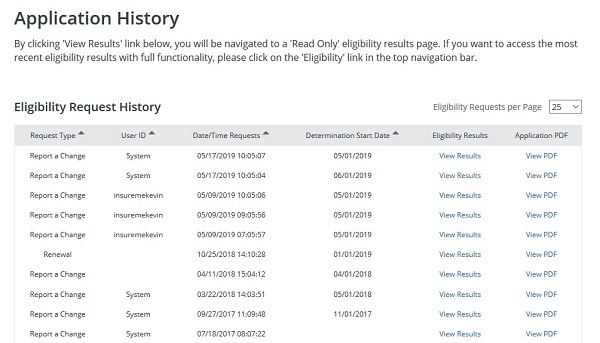
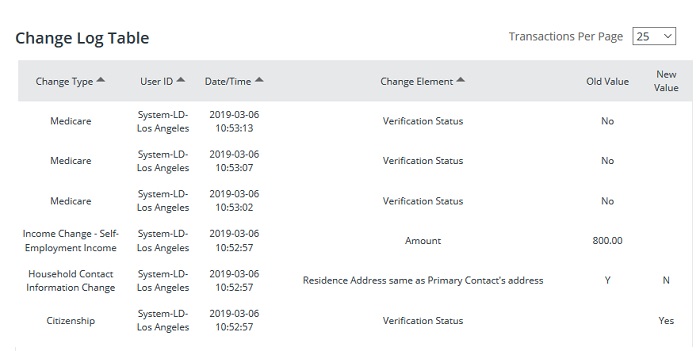
One change that Covered California made several months ago without notifying anyone was to move the transaction history under link View Past Application. This link used to take the user to the Summary page where they could view eligibility, enrollment, transaction history and documents and correspondence. That is all wiped away with the new 19.4 release. The Application History, Eligibility Request History page shows when an application, after any changes have been made, was submitted. It does not show the changes or who made the changes. Sometimes it was nice to know what specific changes were made and by who. All changes to an account are logged by CalHEERS. If this information is still available, it is not readily apparent under the new release.
Prior to the 19.4 update, I could always review the documents and correspondence for an account as an agent. This information was vital to see when letters were sent out and if they were returned to Covered California. It also showed which documents we had uploaded for verification purposes like income or residency. This vital information has been moved to the View Past Application page.
The enrollment dashboard is nice for quick reference. Before, the enrollment information was hidden under the view past application link. The updates make it easier for consumers to see that they can make their first month’s premium payment through the Pay Now button. Plus, the Pay Now button is only active IF the first month’s binder payment has not been made. The health insurance plan will notify Covered California when they have received the binder payment. Covered California will then show the consumer enrolled and Report a Change button becomes active.
Consumers are NOT paying Covered California for their health insurance. The Pay Now button goes to a third-party payment processing webpage. You must have your pop-up blocker turned off for the function to work. The Pay Now button is purely for convenience to assist consumer binding their health insurance with the first month’s premium payment. You can’t make ongoing payments for the health plan through Covered California.
Easier Covered California Health Plan Termination
Covered California has also added a cancel coverage button to the enrollment dashboard now called “Disenroll From Health Plan”. The process for terminating health insurance is much improved. The prior configuration was very confusing with the dates the system was requesting and it would not accept certain dates. Now the consumer can choose, “The Select Termination Date popup displays with a required end date selection as follows:
- Last day of the current month
- Last day of the next month
- Last day of the month after next
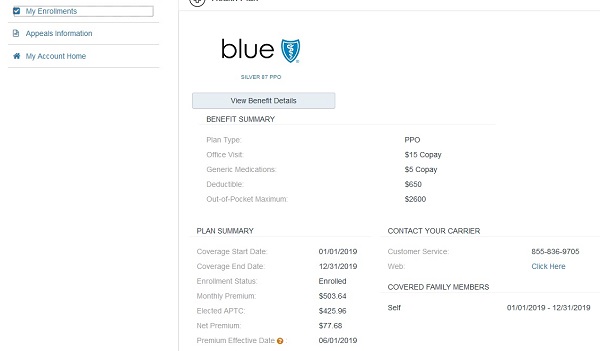
One of my complaints on the My Enrollments page is the gray text. While the pertinent data from the application is in black, the description or title of the field is light gray. Why? Make the text black so we can all read it regardless of what type of device we are using.
Grab Screen Shots Of Changes, Results
The front consumer facing CalHEERS display has been updated, but not necessarily the back end. I had one household where the new enrollment dashboard showed NO APTC subsidy. But when you looked at the individual enrollment, the consumer was receiving a subsidy. Covered California was able to change it, but no one could explain why it showed $0 or why it came back after re-submitting the application. The lesson is ALWAYS take screen shots of changes and results in the Covered California. Since they are making it harder for consumers to track who made changes to the account (Was it the agent, Medi-Cal, Covered California?) you need to be proactive to document account changes.

The new 19.4 release also made changes to Certified Enroller profile page, dashboard, and account features. Currently, the Covered California system has agents like me update our password every three months. That’s good security, but it can be improved. Covered California needs to move to a 2-factor authentication system. Under the 2-factor system, the user would have to put in a unique code sent to him or her either through a text or email.
I have 2-factor deployed for online banking, email system, cloud storage, and website management. It seems like a hassle at first, but you get use to it. It is virtually impossible to hack into any on-line account I have where there is 2-factor authentication activated. You need my mobile phone to either get the text or access the Google Authenticator application. Covered California can harden their system by making agents and other certified enrollers use 2-factor authentication to help protect consumer information.
CalHEERS Updates
Covered California prepared a short 8 minuted YouTube video on some of the changes with release 19.4, you can watch it by clicking the link below.