Does it matter if a person’s sex does not align with their gender identity?
As a Certified Insurance Agent for Covered California I am scrupulous when it comes to reading each question on the application for health insurance exactly as written, except when the Covered California application asks for the sex of the applicant. Instead, I ask for the person’s or dependent’s gender. Covered California should stop asking about a person’s sex and allow them to specify a gender.
Sex versus Gender
Pardon my reluctance as an old guy to say the word sex out loud. Heck, I get uncomfortable when a scene of intimacy between two people flashes across the TV screen. I don’t like asking about the intimate details of a person’s life. While I can be prudish, I’m pretty progressive when it comes to matters of people living out their inherent gender identity.
Sex: either of the two main categories (male and female) into which humans and many other living things are divided on the basis of their reproductive functions.
Gender: the state of being male or female (typically used with reference to social and cultural differences rather than biological ones).
I know some people reading this will think I’m trying to be too politically correct. But that isn’t the inspiration for my request for Covered California to change the question of an applicant’s sex to gender. After helping a variety of individuals and families enroll into health plans through Covered California, I’ve come to appreciate that a person’s biological sex does not necessarily define their gender identity.
Specifically, people who were born intersex had to choose their gender identity at an early age. Some have even changed their public gender identity later in life. In addition, intersex people can face unique health challenges that may be contrary to the gender role they have chosen. Consequently, the biological sex of a person doesn’t really define who they are. The available responses on the Covered California application to the question of sex are either male or female. There is no intersex option.
The biological sex of a person does matter for health insurance and health care purposes. A woman is entitled to no cost preventive mammograms, well woman visits, and birth control. These are specific benefits for females. A transgender man who hasn’t completely transitioned, still needs some of the female health care services to stay healthy and prevent disease. Without the female designation, he may be erroneously denied some no cost services.
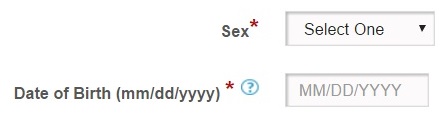
The Covered California application asks for the Sex of each household member. Male and Female are the only options. This is a required response field.
Transgender individuals are fully aware of the limitations of the check boxes for either male or female assignment. They work with their health care providers to understand their health care requirements and how they may not align with the binary choice of male or female.
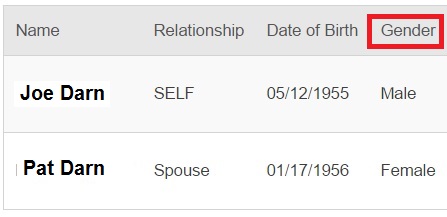
Parts of the Covered California enrollment application data indicates the gender of the household members, not the sex.
From a health insurance rate perspective, there is no longer any differentiation in premium between a male or female individual. The rates are based on age and the location of the residence. Even though the Covered California application asks for the sex of the applicant, in other parts of the data base it is referred to as gender.
We need to move toward applications that allow a person to designate a gender and then let them work with their health care providers to access the appropriate health care services for their bodies. Covered California has a whole optional demographic section on their application that allows people to designate their race. But there is no optional section that allows people to indicate their real gender identity or sexual orientation.
There is a danger in collecting too much information. But if Covered California wants to support their mission of expanding affordable, quality, health care for all its members, more data would be helpful. It’s only through good data on the membership base that will allow Covered California to develop health plans that meet the needs of our state’s individuals and families.