Covered California Health Insurance Exchange
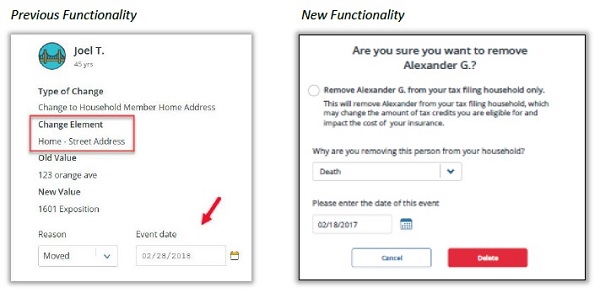
Anyone who has reported just a couple of changes to their Covered California account will remember the multiple questions asking for a reason for the change of each field. Sometimes these reasons on the drop down menu had no relationship to the reason for the change. Consumers, and agents, felt paralyzed that they had to select a reason that was not accurate and then risk being accused of fraud. Covered California with their June 4, 2018, 18.6 release of the enrollment software does away with those perplexing questions.
Fewer Questions When Reporting A Covered California Change Report
In the process of reporting a household change in Covered California could trigger a slew of questions as at the end of the Report A Change function. Just touching a field would trigger a consumer response. When cleaning up account after Medi-Cal had made changes would inevitably lead to numerous reason-for-change questions. If Medi-Cal had entered four or five income entries, and I had to delete most of them, I had to give a reason why each entry was deleted. There was never reason from the drop down menu that it was an erroneous entry.
From conversations with Covered California, they said they did not track the reasons selected for each field change. I think it was a well-intended function to help verify that the change was necessary and to capture data on consumers. In reality, it was a confusing test patients as the consumer or agent had to select reasons for 15 or 20 changes to the application, most of which was just deleting old and erroneous entries.
Covered California says they have removed the type of change reason questions except in the case of removing a household member.
Report a Change Streamlined
The steps for reporting a change in CalHEERS have been significantly reduced. It is no longer required to provide reason and event date information multiple times when reporting a change for your consumer like address change, income updates, etc. Currently, if a household reported a change, the user was prompted to enter the reason and date multiple times, and even when not warranted. This has been updated to only ask reason and date if a household member is to be removed from the application or the plan. If the member is a primary contact or primary tax filer or primary care giver, then an option will be provided to identify a current household member in the role.
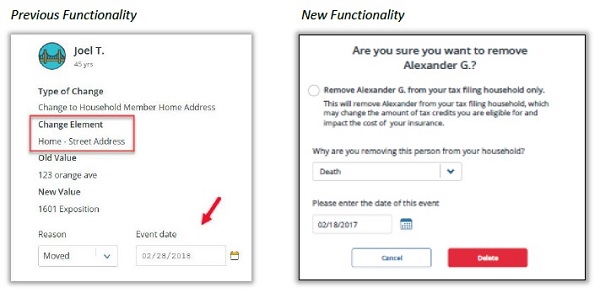
Updated functionality for Report A Change field type changes in Covered California.
The Authorized Representative link has returned as of June 4. There was a lot of confusion about Authorized Representative. It is not for authorizing an agent to assist you with your application that is under Manage Delegates. Authorized Representatives are in case the primary account holder can’t call Covered California because of illness or other reasons. Covered California can release limited data and information to a primary account holder’s authorized representative.
Authorized Representative Link is Back!
This release will restore the Authorized Representative link that was removed in 17.9. It will be returned to the same location under the “More Actions” menu on the consumer Home page. This is used to update or assign another person permission to make changes to the application on the consumer’s behalf.
Covered California also made some changes to the Shop and Compare tool to more closely align with the application. “This new layout offers support for an entire household, or select members, including children and those expecting children. This page now matches the “look and feel” of the rest of the application. It is easier to navigate and find basic information needed by the consumer.”
18.6_CalHEERS_Release_Notes
June 2018 updates to the Covered California online application and shop and compare tool.