Covered California is making minor modifications to their CalHEERS online application for health insurance with the 18.3 program release. The new federal poverty income levels for 2018 will now be active in the system and they are updated the household eligibility page.
Covered California is making minor modifications to their CalHEERS online application for health insurance with the 18.3 program release. The new federal poverty income levels for 2018 will now be active in the system and they are updated the household eligibility page.
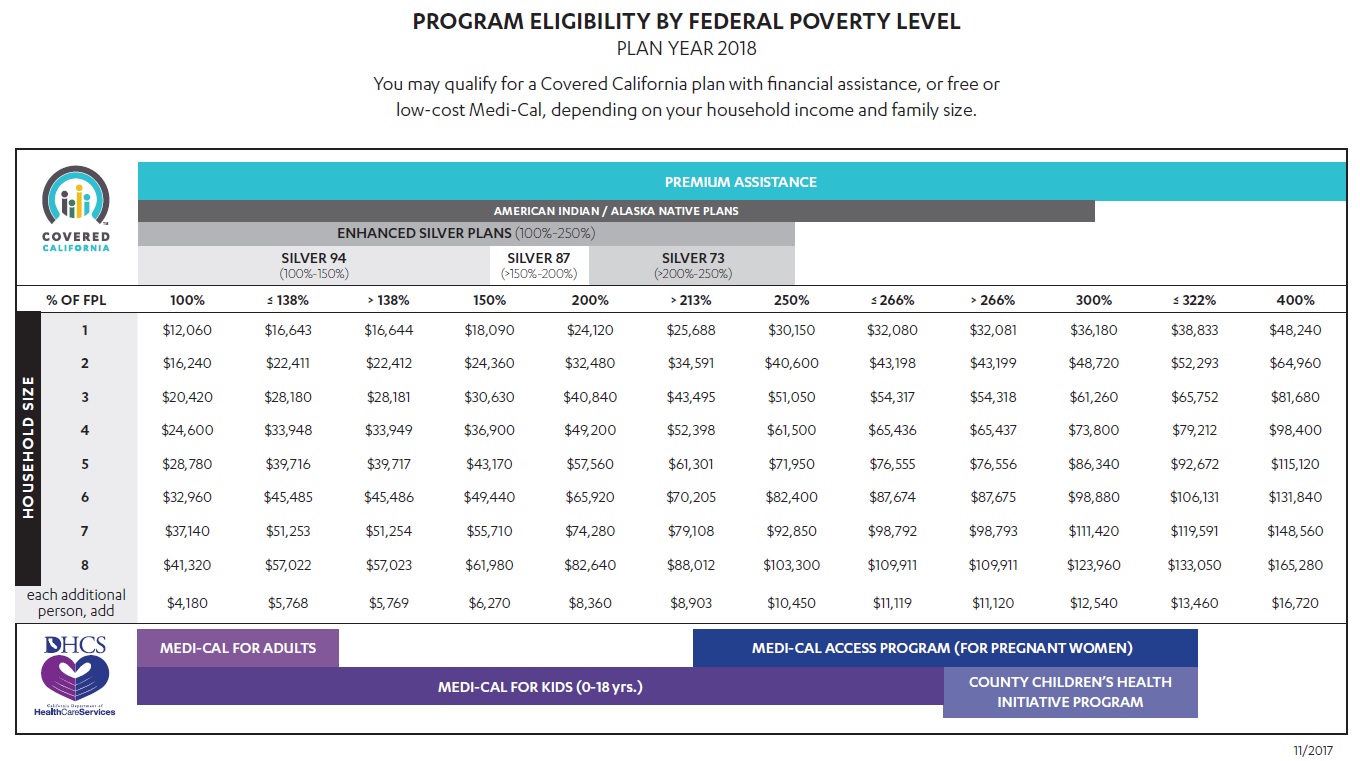
Every year the federal poverty levels based on household income change for program eligibility such as Medi-Cal. Individuals and families who went through Covered California for the 2018 plan year came were subject to the 2017 federal poverty levels.
Federal Poverty Level Guidelines for Medi-Cal Determinations
The 2018 Federal Poverty Level (FPL) guidelines will be incorporated into CalHEERS to reflect new values for Medi-Cal consumers with this release. CalHEERS uses the FPL guidelines to determine eligibility for Insurance Affordability programs such as Medi-Cal, Applied Tax Credits (APTC) and Cost Sharing Reductions (CSR).
2018 FPL guidelines are updated for Medi-Cal determinations only and will not affect eligibility for Covered California consumers. The Covered California 2017 levels are used for the 2018 benefit year.
The table will be effective from 01/01/2018 forward and any Covered California consumer previously given APTC/CSR eligibility who reports a change, will be reevaluated for eligibility and may find that they now qualify for Medi-Cal using the updated 2018 FPL table. – CalHEERS 18.2 Release Notes
Covered California has also updated the eligibility page so it looks like the rest of household member avatar centric profile picture. Now, if your daughter’s Covered California cartoon avatar is a depiction of the Golden Gate Bridge, that same cute picture will be displayed on the household eligibility results summary page.
Updated Eligibility Results Page
Once an application has been completed and submitted, the consumer or enroller will see the enhanced “Household Eligibility Results Summary” page. This page now matches the “look and feel” of the rest of the application. It is easier to navigate and find basic information needed by the consumer.
- The “Household Member” column lists all members who are enrolling.
- “Program Eligibility” lists the member’s qualified programs.
- “Action Required” displays “Yes” when the consumer needs to take additional steps to finalize their eligibility.
The “View” button links to additional details. If documents are required, the document type and deadline will be shown.
- “Application Request Log” is only viewable to enrollers, not the consumer.
- “View PDF” downloads a copy of the application.
- “View Budget Worksheet” link displays the criteria used in making the determination.
Updated Interface for Enrollment Grouping
Each household member is displayed in an enrollment group based on their eligibility results. The grouping options have not changed, but the layout is easier to understand and navigate both for consumers and enrollers. Examples of an enrollment group could include:
- A household member with a Covered California Plan with premium assistance.
- Household members with premium assistance and American Indian/Alaska Native cost sharing reduction.
- Household member who have a county enrollment.
Enrollment Grouping Quick Guide
The custom grouping functionality has been enhanced to reflect the new look of the application. Additional messaging has been incorporated to ensure enrollers can assist consumers with making the best choice for their household. – CalHEERS Release Notes 18.3
Enhanced Messaging for Enrollment Grouping
The Choose Enrollment Groups page displays after the consumer submits an application for coverage and then reaches the Household Eligibility Results Summary page.
The application will group household members into separate groups based on unsubsidized, subsidized, American Indian/Alaska Native or Medi-Cal eligible groupings. The first choice displayed is always the recommended grouping.
Examples of an enrollment group could include:
- Household members with Advanced Premium Tax Credits (APTC) with American Indian/Alaska Native Cost-Sharing Reduction. See “Dan” in the picture.
- A household member with a Covered California Plan with Advanced Premium Tax Credits. See “Thao” in the picture.
- Household members who have a County Enrollment whether for regular Medi-Cal or Medi-Cal Access Program (MCAP) or another program. See “Child” in the picture
The system first displays the Recommended grouping for the consumers. You can modify the groupings to fit the consumer’s situation. When the consumer wants to modify the grouping, you can click the “Edit Groups” button. The following screen shows as a pop-up when you select the “Edit Groups” button.
- “One Plan for All” means that consumers who qualify for the same programs will be grouped together for enrollment into the same plan. Note that County-only eligible members cannot be grouped with Covered California members.
- “By Individual” groups each household member in their own group. Plan selection will be chosen one at a time for each consumer.
- The “Custom” grouping allows household members to be in a separate group based on the individual situation, such as when a doctor is only available in a specific plan.
Note: If you need to change the groups, it must be done prior to enrolling in a plan. The system provides easy to follow steps for re-grouping the household members.
While the application does allow for customized grouping, there are new messages that will display if the grouping results in higher costs or reduction in benefits. The “Important Considerations before Regrouping” message displays as a notification that the initial suggested enrollment grouping is usually the most beneficial to the consumer.
Another example of this message is in the event the household has American Indian/Alaskan Native household members.
The “Important Considerations before Regrouping” message specifically calls out when an American Indian/Alaskan Native household member is grouped with other family members. In this situation, the extra benefits of lower out of pocket payments for the American Indian/Alaska Native member will not be a part of the new grouping, so the household cost will rise.
If a consumer decides to proceed with this grouping, another message will be displayed on the enrollment grouping page like the one pictured below. It is important to note that it is the consumer’s choice to proceed with the least beneficial grouping.
After confirming the enrollment grouping of choice, the Enrollment Grouping page will display the household members by group, with the APTC that each group qualifies. They are then prompted to proceed with plan selection by selecting the “Choose Helath Plan” button. – Enrollment Grouping Release Notes Quick Guide
The secure mail box has been updated and access to it will now be shown under the More Actions column at the bottom of the Covered California home page. There are new buttons to archive messages and an exclamation point for high priority like you are about to lose your premium tax credit subsidy if you do not provide proof of income.
Where Is The Summary Page?
The 18.3 changes how agents and consumers find the Summary page. Before you could click on View Eligibility Results and on the left sidebar would be the nested pages under Summary. Covered California changed this path. They have added View Past Applications link under the More Actions column on the home page. This will get you to the Summary page that has the Documents and Correspondence and Current Enrollment pages, along with the Transaction History.
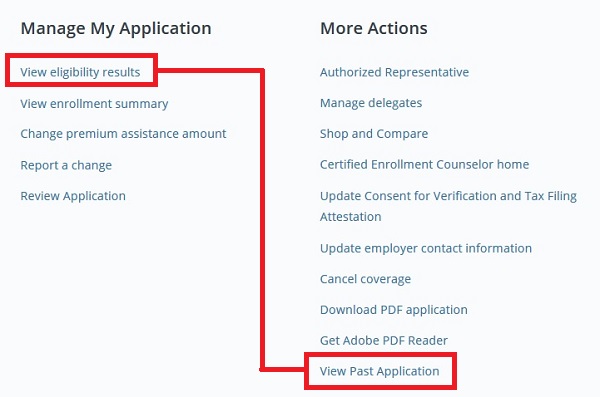
Update 18.3 changes how agents and consumer get to the Summary Page. View Past Application will get you to a page with the other summary pages.