 As Covered California ramps up for open enrollment for their “premium assistance” eligible health insurance plans starting in October, Julie Wiegand of Covered California declared they need “boots on the ground” in the form of Certified Enrollment Counselors. Formerly known as Assisters, Certified Enrollment Counselors (CEC) are expected to play a significant part with enrollment in many different communities. The latest webinar about the In-Person Assistance Program, where organizations are paid to enroll individuals and families, was the grand start of Covered California’s recruitment, training and certification drive.
As Covered California ramps up for open enrollment for their “premium assistance” eligible health insurance plans starting in October, Julie Wiegand of Covered California declared they need “boots on the ground” in the form of Certified Enrollment Counselors. Formerly known as Assisters, Certified Enrollment Counselors (CEC) are expected to play a significant part with enrollment in many different communities. The latest webinar about the In-Person Assistance Program, where organizations are paid to enroll individuals and families, was the grand start of Covered California’s recruitment, training and certification drive.
Assistance from “Boots on the ground”
The creation of the In-Person Assistance Program which encompasses Certified Enrollment Entities (CEE) managing Certified Enrollment Counselors confirms the old adage of “It’s never as easy as it looks”. Hobbled by arcane bureaucratic regulations of the Affordable Care Act and California state law, the In-Person Assistance Program is more cumbersome than most people may realize. It’s unfortunate that the final assistance program is just complicated enough to potentially drive away people who have the time and desire to enroll families, but don’t want to go through the meat grinder of government regulations.
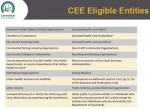
Certified Enrollment Entity may fall to government
Before any Assisters or Certified Enrollment Counselors can put their “boots on ground” to enroll Californians, they have to be affiliated with a Certified Enrollment Entity. As of September 6th, Covered California only had a couple CEEs cleared to recruit and manage CECs. A variety of organizations from Chamber of Commerce’s to school districts are eligible to become a CEE. The CEE will be the organizations that actually receives the $58 compensation for each household that is enrolled and has the policy activated in January, 2014.
All aboard the Enrollment train
The forty-nine page CEE contractual agreement is enough to scare off many nonprofits from participating (Download at end of post). Another hurdle is the expertise necessary to manage a payment system for the affiliated CECs, issuing 1099’s and grappling with liability insurance issues to the organization. My fear is that the obstacles and head aches are so numerous to becoming a CEE; the only participants will be government institutions who recruit employees to be CECs.
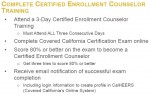
Certifying counselors and assisters
The contractual agreement the Certified Enrollment Counselor is far less daunting than the CEE at only 13 pages. Big challenges for the CEC are getting through the 2 1/2 day training, tests and the finger-printing background check. Aside from enrolling people because you believe in Obamacare, the compensation may or may not prove to be an incentive. With less than a month before open enrollment, you could hear a twinge of anxiety from the folks at Covered California that the whole In-Person Assistance Program had gotten off to a slow start. They need people who can get out in the community and enroll families, at least that’s the plan.
Monetary compensation is a gamble
The $58 successful enrollment compensation, which is paid to the CEE and not the CEC, won’t begin until sometime in January. That means a couple months of potentially solid work with out any reimbursement for the counselors. On the other hand, the CEE might advance a partial payment to the CEC on the gamble that the household enrolled will stay in the program. If a family decides not to participate or doesn’t pay the premium, the $58 compensation isn’t paid to the CEE.
At the mercy of the CEE
The CEE is not under any obligation to pay the CEC the full $58 compensation amount they receive from Covered California that I could find in the agreement. Consequently, some CEEs may pass through the $58 per enrollment or deduct a portion for administration. As an incentive to be a full service enrollment administrator, the CECs will be compensated $58 for households enrolled in Medi-Cal.
Face to Face, no telephone enrollments
There is the potential for a bottle neck in the overall enrollment if there are not enough CECs to serve various populations through out California. The CECs must meet with the individual or family in-person. Enrollment that is to be compensated can’t be over the phone. The burden of in-person assistance may fall on local governments, school districts, or clinics if there are not enough CEEs with the requisite “boots on the ground” CEC’s to meet the enrollment demand.
No law prevents helping neighbors enroll
However, don’t let the bureaucratic nightmare of forms, contacts and compensation dampen your enthusiasm for guarantee issue

You don’t need an official government show to help your neighbor.
affordable health insurance for all Californian’s. There is no law or regulation that prohibits people from helping their neighbors, family and community members with enrollment assistance. Perhaps you are a church with several computers that can be used by the community. Recruit folks with some computer knowledge, read up on the Covered California enrollment system and then open the doors. If Covered California can’t give you some background, I’ll give you an overview.
We can’t rely on government boots
The Affordable Care Act or Obamacare is to important to our country to let it falter because people are under the impression that only the government can help individuals and families enroll. No! This is about our communities. Help your neighbors enroll if you can. We do need “boots on the ground”, but tennis shoes will work just as well.
Link to Certified Enrollment Entity website
[wpdm_file id=98 title=”true” desc=”true” template=”bluebox ” ]
[wpdm_file id=99 title=”true” desc=”true” template=”bluebox ” ]
[wpdm_file id=100 title=”true” desc=”true” template=”bluebox ” ]