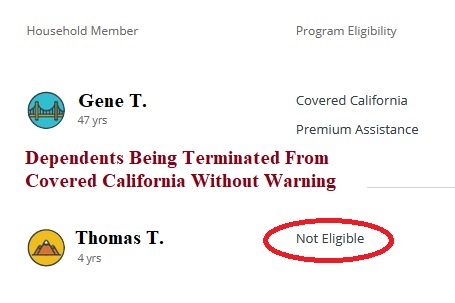
Covered California seems to have a small but consequential issue where dependents have been kicked-off of the family plan and left with no health insurance. All of the cases I am aware have occurred during Covered California’s implementation of the larger subsidies authorized by the American Rescue Plan. The significant and consequential problem with the termination of the dependent’s plan is that the affected individual was NOT enrolled in Medi-Cal, or even in a private plan with no subsidy. The children are just left without health insurance.
No Warning of Child’s Health Plan Termination
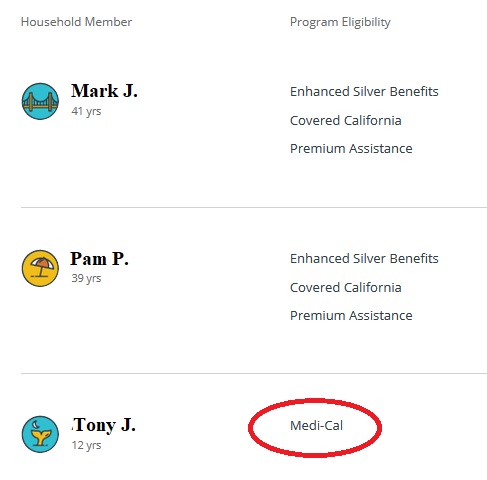
The loss of enrollment in a private plan with the subsidies under this latest glitch is different from the usual termination that places the child into Medi-Cal. If the household income falls below 266 percent of the federal poverty level, then all dependents 18 years old and younger are determined eligible for Medi-Cal. When this happens, Covered California notes Medi-Cal eligibility and pushes the enrollment information over to the county of residence for final Medi-Cal eligibility determination and enrollment.
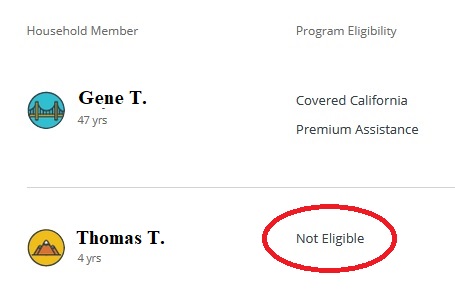
The latest round of terminations happened with no warning and the eligibility results show Not Eligible. The Not Eligible result indicates that the dependents information is not being forwarded to Medi-Cal. The child effectively has no health insurance. There is no offer to enroll the child in a health plan without the subsidies. The Covered California system seems to be treating the child as if they have other coverage such as from an employer or Medicare. When you indicate a household member has Medicare, the eligibility results show Not Eligible for Covered California participation.
Children Were Eligible During Open Enrollment
What is truly odd is that all of the dependents I know of who have been booted off the family plan were renewed by Covered California during Open Enrollment in 2020 and were receiving a subsidy to lower the cost of health insurance. What happened in four months to make these children not eligible for Covered California? All of this started when Covered California updated their online application and enrollment system (CalHEERS) to implement the larger subsidies of the American Rescue Plan. Covered California even notified me that some households had to increase their income or risk being put into Medi-Cal. All of the families I am familiar with whose child was terminated had incomes above all of the Medi-Cal limits.
The one common denominator between all of the households is that at some point the child was in the Medi-Cal system. What this tells me is that Covered California is picking up on some Medi-Cal database (SAWS or MEDS), assuming the child has active Medi-Cal enrollment, and terminating the child’s health plan.
What is most distressing to parents is that they are learning of the loss of coverage from their health plans, not Covered California. One account showed the child was still eligible for health insurance through Covered California through May, but the carrier had sent a notice of termination for April 30th. Covered California sends out all sorts of confusing letters when a household first enrolls for health insurance. They can at least add a letter informing the household that a child is being terminated from coverage.
The only recourse Covered California has offered is that the parent needs to contact their county Medi-Cal office to straighten out the mess that they created. Of course, this little issue probably only affects a tiny fraction of the Covered California enrollment. Nonetheless, parents don’t like surprises such as learning their children no longer have any health insurance.