For adults in California who have been diagnosed with HIV or AIDS, there are programs to help pay health insurance premiums, healthcare costs, and prescription medications. Both the health insurance premium and drug assistance programs are administered by the California Department of Public Health.

Health insurance premium assistance is handled by Office of AIDS. The program can help pay for health insurance premiums and some health care costs when the applicant is enrolled in AIDS Drug Assistance Program (ADAP.) The first step to getting help for the health insurance premiums to apply for ADAP. In addition to being eligible for ADAP, the applicant must be enrolled in a creditable health plan and not have full-scope Medi-Cal.
The Office of AIDS – Health Insurance Premium Payment (OA-HIPP) assistance can help with paying for health plans from
- Individual and Family Plans, including Covered California
- Medicare
- Employer Sponsored health insurance.
Individual and Family, Covered California Health Plans
For off-exchange individual and family plans, purchased directly from the health plan, OA-HIPP will send a payment directly to the health plan. If you are enrolled through Covered California and receive a subsidy, OA-HIPP will pay your portion of the premium payment, after any subsidy, directly to the health plan.
Medicare Premium Assistance
If you are a Medicare beneficiary, the Medicare Premium Payment Program (MPPP) can help cover premiums of a Medicare Advantage plan, Part D prescription drug plan, and Medicare Supplement plans. The Medicare premium assistance cannot cover the Part B premiums of Original Medicare. The premium payment is sent directly to the plan sponsor. If you are fully dual eligible, Medi-Medi, there will be no assistance.
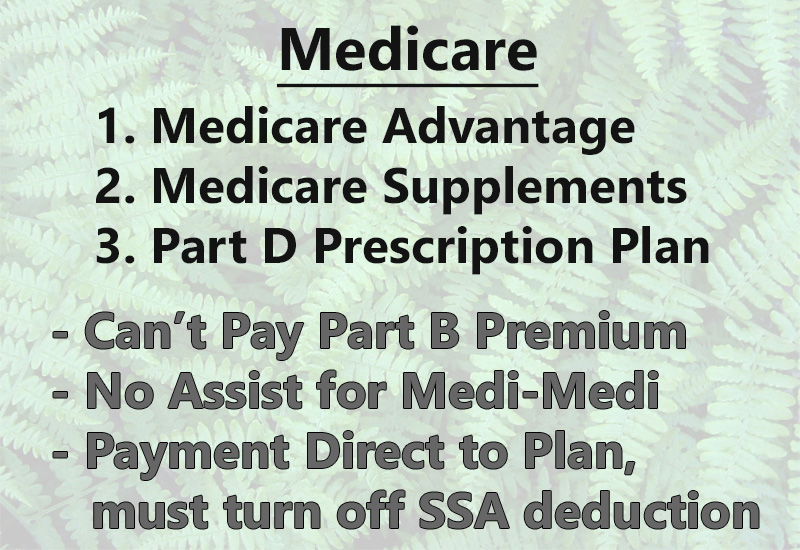
However, the Medicare program can cover certain out-of-pocket costs associated with Medicare Advantage plans that may not be covered by Medi-Cal. If you have your Medicare Advantage or Part D drug plan premiums deducted from your Social Security direct deposit, you will have to request direct billing from the stop the SSA deduction. You may not be able to do this until the next Annual Enrollment Period. Then the program can pay those premiums directly.
Employer Sponsored Health Insurance Premium Assistance
Employer sponsored plans are reimbursed differently. The program pays the employer the amount of the health insurance that had been withheld from the employee’s payroll deposit. The employer then reimburses the employee. The reimbursement system can be challenging for a small business. In addition, some employees may not want their employer to know about their HIV positive health status.
Out-of-Pocket Health Care Expenses
All of the categories of health insurance premium assistance – Individual and Family, Medicare, Employer Sponsored – can also help with out-of-pocket health care expenses. The programs will cover expenses that accrue to meeting the maximum out-of-pocket amount of the health plan. These costs include copayments, coinsurance, and deductibles, all of which add towards the maximum out-of-pocket amount.
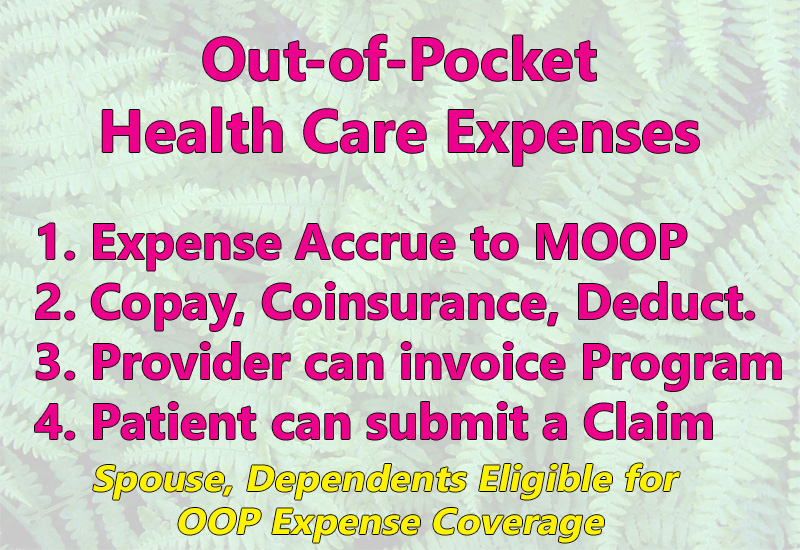
Individuals enrolled in the AIDS Drug Assistance Program (ADAP) and enrolled in the premium assistance program receive member identification card. This ID card is shown to the provider at the time of the appointment. Reimbursement is directly to the provider. If the patient had already paid for the health care service, the provider reimburses the patient or applies a credit to their account. Spouses and dependents of the ADAP individual can also receive assistance with their out-of-pocket health care costs.
Dental and Vision Insurance Premium Assistance
Dental and vision insurance premiums may also be covered by the programs. The individual must be enrolled in the health insurance premium assistance program. Vision premiums can only be covered if they are included as part of a dental or health plan. However, dental and vision costs are not covered by the Medicare Premium Payment Program.
AIDS Drug Assistance Program (ADAP)
The first step toward having the California Department of Public Health assistance in covering health insurance premiums and out-of-pocket health care costs is applying for the AIDS Drug Assistance Program (ADAP).
In order to qualify for ADAP you must:
- Be a California resident
- Be HIV positive or AIDS diagnosis
- At least 18 years of age
- Not have a Modified Adjusted Gross Income greater than 500 percent of the federal poverty level for the household size
- Not have full scope Medi-Cal or other third-party payers for drug coverage
ADAP will cover the cost of FDA approved medications used in the treatment and suppression of HIV and AIDS. The ADAP office has trained enrollment counselors to assist with filling out the application. You must apply in person at one of many locations throughout the state. Eligibility is reviewed annually, and certain forms must be completed and submitted 45 days prior to the applicant’s birthday. The ADAP application will ask if the applicant wants to participate in the health insurance premium assistance program.


