One of the great features of the Affordable Care Act is the expanded types of preventive office visits at no charge like screenings for cancer. In addition to mammograms, the fairly invasive procedure of a colonoscopy for adults over 50 years of age is also supposed to be covered at no charge, no deductible, no copay and no coinsurance. Unfortunately, for a variety of reasons, people are getting invoiced from insurance companies and then having to fight to have the charges removed.
Detailed Report
The confusion over the colonoscopy billing is detailed in a new report Coverage of Colonoscopies Under the Affordable Care Act’s Prevention Benefit jointly authored by The Henry J. Kaiser Family Foundation, American Cancer Society and National Colorectal Cancer Roundatable.
Download full report here ->[download id=”31″]
A visit to the doctor can be broadly broken down into three categories.
- Preventive: like a yearly physical, vaccination or consultation for an issue.
- Diagnostic: when you see your physician to diagnose a pain or rash or other problem.
- Therapeutic: such as when the doctor, physician’s assistant or nurse stitches up a cut, freezes a wart or rinses out ear wax.
It is not uncommon for a preventive visit to morph into a diagnostic visit resulting in a therapeutic action. It is these definitions and actions that are giving the doctor’s office and insurance companies difficulties when it comes time to generate billing codes for record and insurance purposes.
Splitting hairs and cost sharing
The report found that patients can be unexpectantly billed for cost-sharing of a colonoscopy under three scenarios.
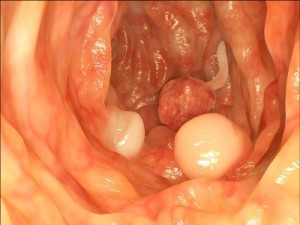
- When a polyp is detected and removed.
- When a colonoscopy is performed after a positive lab result.
- Individuals at increased risk for colorectal cancer receiving more frequent colonoscopies.
Gutteral view
From all indications, the ACA regarded at least the first colonoscopy at age 50 completely
preventive even if benign or cancerous polyps were removed during the procedure. However, some insurers are viewing the removal of any polyp as a therapeutic action and therefore subject to cost sharing. Yet, a medical director for one insurance company is quoted as saying, “[Polyp removal] is exactly why you’re doing this…if you take that polyp out, you have prevented cancer.” The report went on to mention that this particular insurance company did impose cost-sharing if a specific code was not used by the provider.
Therapy or prevention
A real gray area for both providers of colonoscopies and insurance companies is cost sharing for the colonoscopies as a follow-up to a positive fecal occult blood test (FOBT). If the FOBT is positive for blood in the stool, a colonoscopy is recommended to determine the source of the blood which could be from cancerous colorectal polyps.
Which comes first the pain or the problem
Similar to the issue of higher frequency colonoscopies for people at high risk of cancer, follow-up colonoscopies have different variables such as age and history that lead insurance companies to determine the colonoscopy is diagnostic or therapeutic and not preventive. If it is not coded or accepted as preventive, the insurance company will impose cost sharing to the member. The report notes that several states are working on legislation to clear up the issues of cost sharing on colonoscopies.
Demand prevention at no cost
If you are 50 year old and are scheduling a colonoscopy, you should repeatedly remind your doctor’s office and the out-patient clinic that performs the procedure that it’s preventive and not subject to cost sharing of any type. If you are unsure of your particular situation, contact your doctor and insurance company for clarification. If you get 2 different answers, which are entirely possible, contact your states department of insurance to get a determination.
______________________________________________________________________________
[schema type=”review” name=”Insurance companies find dollars in your colonoscopy” description=”Synopsis of findings of cost sharing problems with no cost preventive colonoscopies, providers and insurance companies. The Henry J. Kaiser Family Foundation, American Cancer Society, National Colorectal Cancer Roundtable” rev_name=”Coverage of colonoscopies under the Affordable Care Act’s prevention benefit” author=”Kevin Knauss” pubdate=”2012-09-21″ ]