 Ms. B had been faithfully making her premium payments for her Kaiser health plan she purchased through Covered California during open enrollment in 2014. When she went to use her health plan, Kaiser told her that the plan was not active. But the enrollment summary of her Covered California account shows she is enrolled. It seems that Kaiser has been accepting not only her premium payments but potentially the tax credits from Covered California for a health plan that is not enforce.
Ms. B had been faithfully making her premium payments for her Kaiser health plan she purchased through Covered California during open enrollment in 2014. When she went to use her health plan, Kaiser told her that the plan was not active. But the enrollment summary of her Covered California account shows she is enrolled. It seems that Kaiser has been accepting not only her premium payments but potentially the tax credits from Covered California for a health plan that is not enforce.
Kaiser accepted the premium payments and the tax credits?
Kaiser has no record of Ms. B ever making any payment toward her health insurance as of September 30, 2014. As is often the case in a bureaucratic melt down, the onus to prove Ms. B had been making her health plan premiums has been placed on her shoulders by Kaiser and Covered California. This is regardless of the fact that their respective systems failed to catch the transfer of payments without a credible health plan in place. The absurdity of this situation is further exacerbated by the lack of assistance in resolving the issue by any of these giant organizations.
She paid without ever receiving an invoice
Ms. B never received any correspondence from Kaiser beyond the first letter instructing her where to send her payment for her first month’s premium amount. With the ensuing chaos that many of the health plans were having getting proper invoices out to new members, there wasn’t much thought given that she had not received a bill for subsequent months. She continued to send payments to the same address in Pasadena, CA assuming that her premium payments would be properly credited to her account.
She couldn’t ride the train, even though she paid the fare
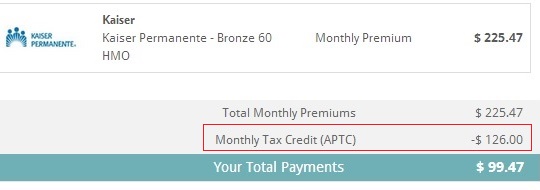
Kaiser should be receiving $126 per month for a plan that isn’t active.
Because Ms. B had been a Kaiser member before, she knew that she would always have the same member ID number and she still had her old card. When she went for her annual well woman check-up she learned that her plan was not active, she was no longer a member. How could this be? She had been making her payments in good faith even without receiving an invoice. She has the cancelled checks to prove it.
No payment equals automatic cancellation
When a prospective member doesn’t make their binder payment for their first month’s premium or stops making any premium payments and is dropped from the plan, the health insurance company is supposed to notify Covered California. When the member is cancelled Covered California will stop sending the estimated Advance Premium Tax Credit to the health insurance company. As Ms. B’s agent, I looked at her account at Covered California and she was still showing as being enrolled in the Kaiser plan. It is therefore assumed that Covered California was still advancing the tax credit to Kaiser on her behalf.
Has Covered California been audited?
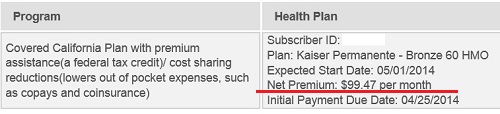
Covered California enrollment summary shows the health plan still active, not cancelled.
I haven’t been able to learn if Covered California performs any internal audits of their accounts with the carriers. It hasn’t been explained if a carrier like Kaiser sends a statement to Covered California to be reconciled or if there is another mechanism to verify the correct advance premium tax payments. At this point, it looks as if Kaiser has received both the premium payments from Ms. B and the advance tax payments from Covered California. We do know that Kaiser is demanding Ms. B send copies of all her cancelled checks to prove she was making her premium payments.
Plans, but no customer service
Covered California is good at marketing their plans but they fail to help consumers navigate the challenges presented by the bureaucratic billing systems of the carriers. Within the contract between Covered California and carriers, the contractors or health plans are expected to provide superior customer service.
3.18 Customer Service.
Contractor acknowledges that superior customer service is a priority of the Exchange. Contractor shall work closely with the Exchange in an effort to ensure that the needs of the Exchange Enrollees are met. Contractor shall provide and maintain all processes and systems required to ensure customer service, record protection and uninterrupted service to the Exchange and Contractor’s Enrollees in the Exchange in accordance with the standards set forth at Attachment 6 (“Customer Service Standards”), applicable laws, rules and regulations, including, those consumer assistance tools and programs required to be offered through the Exchange as set forth at 45 C.F.R. § 155.205 and 45 C.F.R. § 155.210.
Yet, neither Covered California nor Kaiser is offering superior or even adequate customer service. What they excel at is pointing their finger at one another and telling consumers they have to contact the other guy. All this leaves Ms. B to prove she’s not the bad actor in this poorly produced theatrical production of Covered California.
IT failure
When the Affordable Care Act was first introduced there was anxious debate over how to prevent ineligible citizens and non-citizens from benefiting from the Advance Premium Tax Credits. Perhaps overlooked was how the health insurance companies might receive the advanced subsidies when they weren’t entitled to them. While this situation is a prime example of the unprepared and untested IT systems put in place to facilitate the transfer of the tax credits, you have to wonder how many other carriers are being paid for non-existent health plan members.
[wpfilebase tag=file id=160 /]


