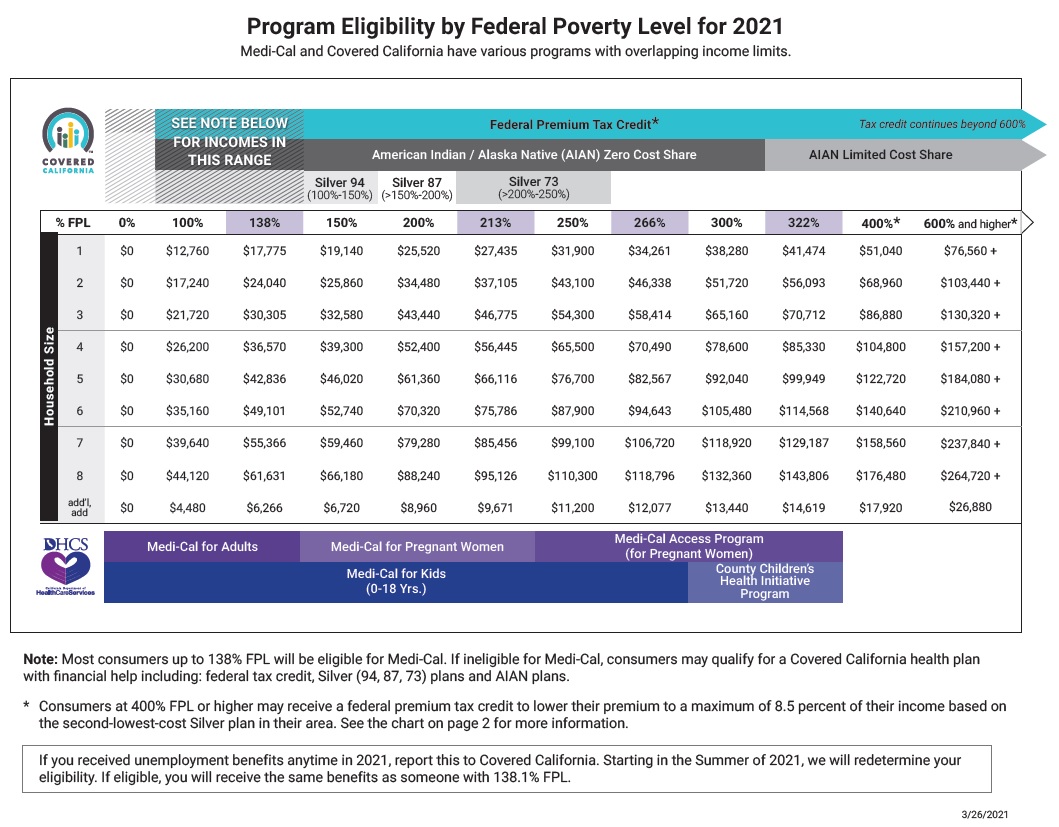
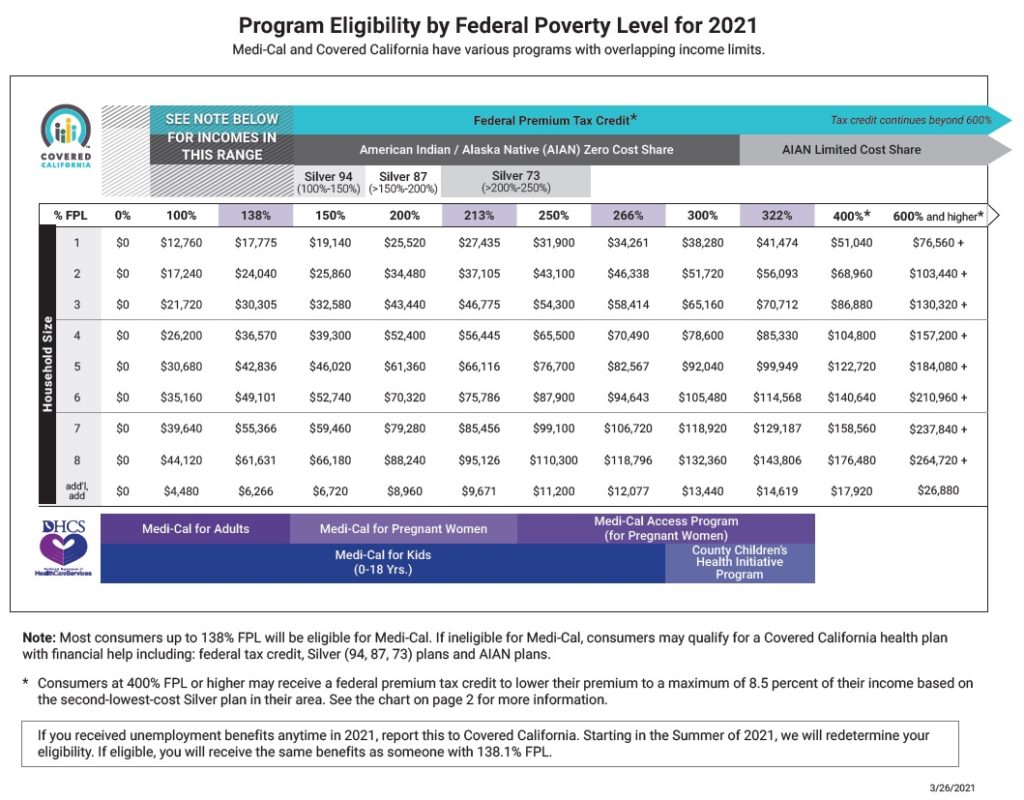
With the passage of the American Rescue Plan that changed the subsidy levels, Covered California has issued a revised income and eligibility table for 2021. With the implementation of the American Rescue Plan, some Covered California consumers may get bumped into Medi-Cal.
Larger Subsidies or Medi-Cal Await Covered California Update
The income ranges in the revised table did not change because they were based on the already released 2021 federal poverty levels for income. What has changed is that the California Premium Assistance Subsidy is no longer listed. This is because the new federal Premium Tax Credit subsidies are larger than anything California was offering. Also note that the Federal Premium Tax Credit extends beyond 600 percent of the federal poverty level.
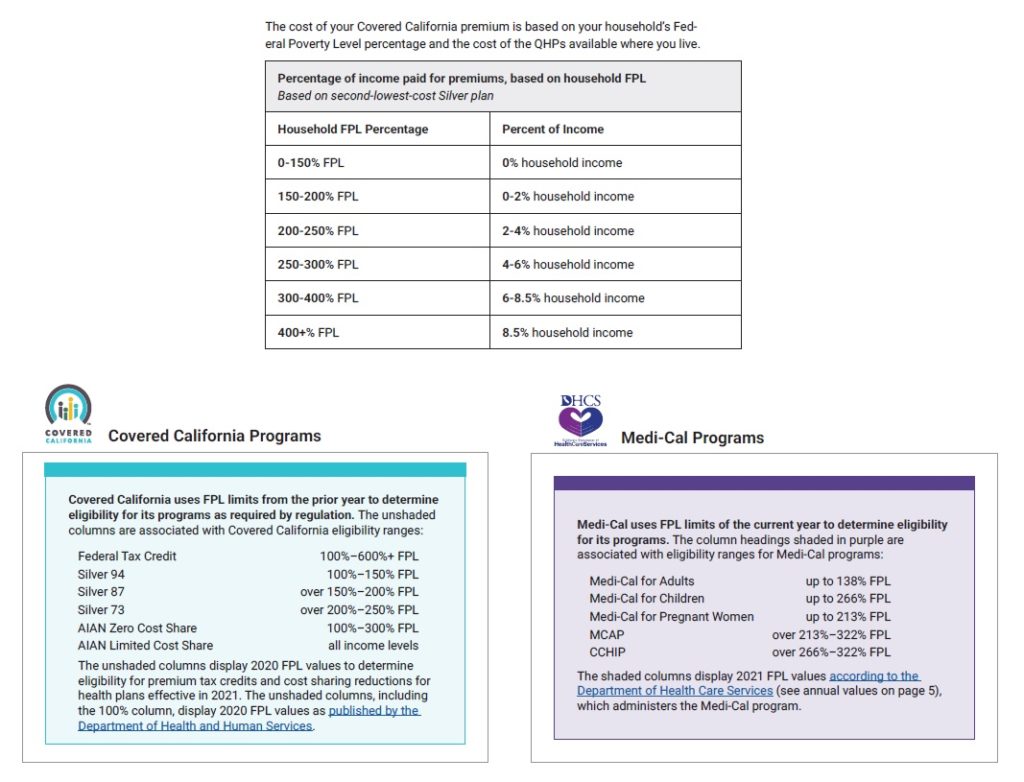
The eligibility income percentages for the enhanced Silver plans (94, 87, 73) did not change nor did income percentages for expanded Medi-Cal eligibility. What has been updated, based on the American Rescue Plan, is the household contribution percentage relative to the Second Lowest Cost Silver Plan in the consumers region. All of those percentages have been reduced. For household incomes up to 150 percent of the federal poverty level, it is now at a zero percent contribution. This means the subsidy amount will be equal to the Second Lowest Cost Silver Plan.
Update Income To Avoid Medi-Cal Enrollment
Normally, when a consumer enrolls into a Covered California health plan with the subsidies during open enrollment, nothing changes for the entire year. However, if a consumer makes an update to their application (change of address, removing a family member, change of income) the entire application is reviewed for eligibility. If the federal poverty level income ranges have changed since the initial application, and the income level is in the Medi-Cal range after the consumer’s update, the household is determined eligible for Medi-Cal and put in a Carry Forward status.
With the American Rescue Plan updates to the Covered California system, all consumers will be reviewed for enhanced subsidy benefits. Unfortunately, this review or refresh is like resubmitting the application for eligibility determination. That means that if the income of a consumer is now below the Medi-Cal line, because the federal poverty levels have increased for 2021, they will be put into the Carry Forward status.
Covered California is advising consumers whose income is close to 138 percent of the FPL for adults and 266 percent FPL for children, to carefully review and adjust their income if necessary, to avoid the Medi-Cal determination. The Covered California update is set to happen April 12th.
2021 Income Table ARP CoveredCa_March Revised
Covered California income table reflecting the enhanced subsidy percentages under the American Rescue Plan Act, March 2021.