The standard benefit design individual and family health plans in California for 2024 mostly contain surprise bills. Outlined within the Evidence of Coverage documents are the details that can cause unexpected health care costs. While some plans may have no medical deductible, there can be coinsurance for health care services.
Coinsurance in a health plan is when the member is responsible for a certain percentage of a health care service cost either before or after a medical deductible. Most health plans will offer some health care services at a set copayment or fixed cost, this includes prescription medications. The Silver through Platinum plans have a large list of services subject to a copayment, not subject to meeting any medical deductible.
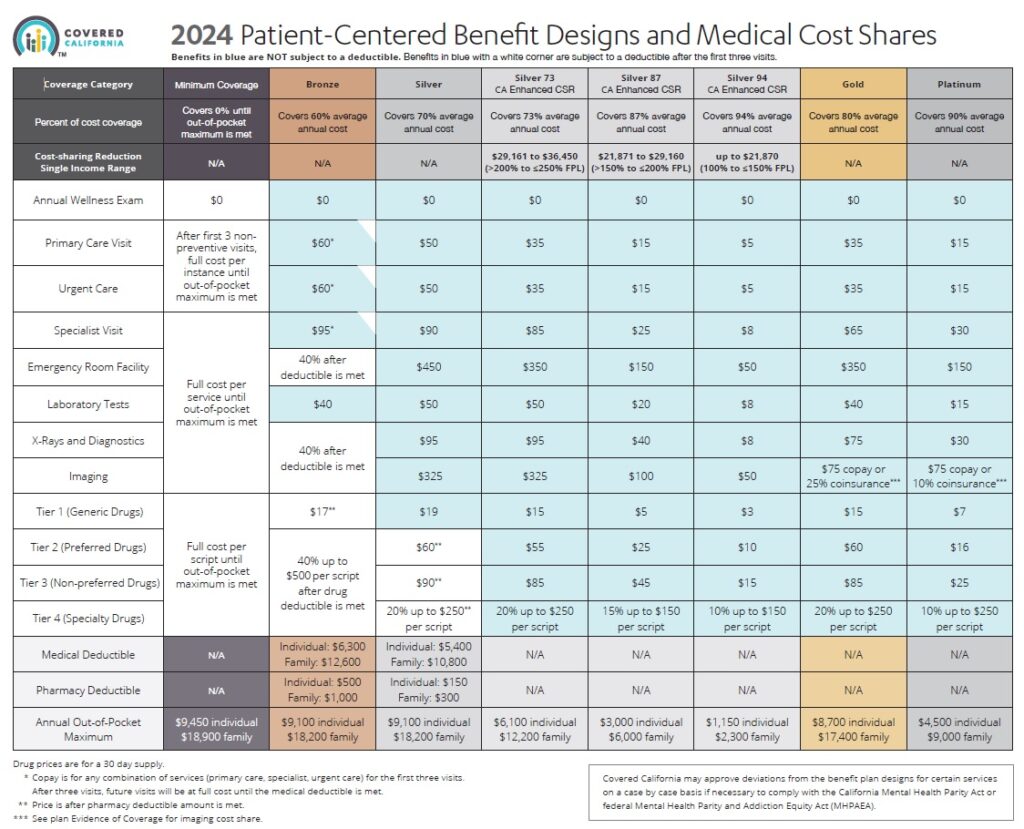
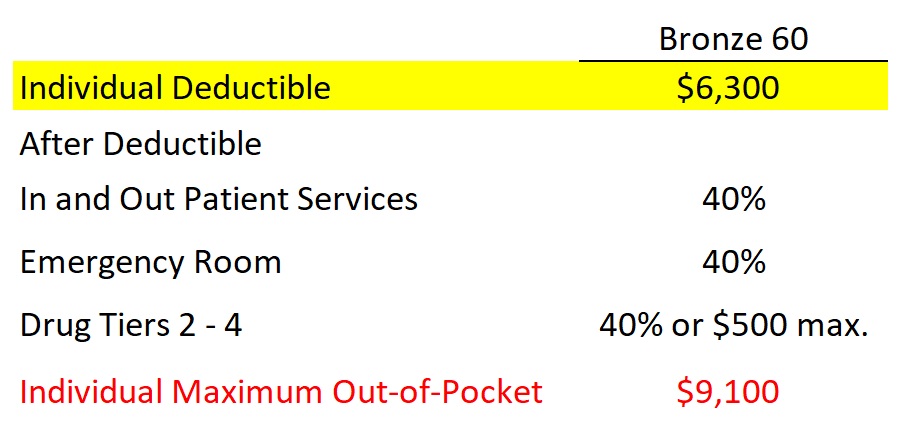
Except for a few office visits and labs, under the Bronze plan, you must pay the full negotiated cost of the health care service until you meet the deductible of $6,300. The next dollar over $6,300, you pay $0.40 and the health plan pays $0.60 until you meet the maximum out-of-pocket amount of $9,100.
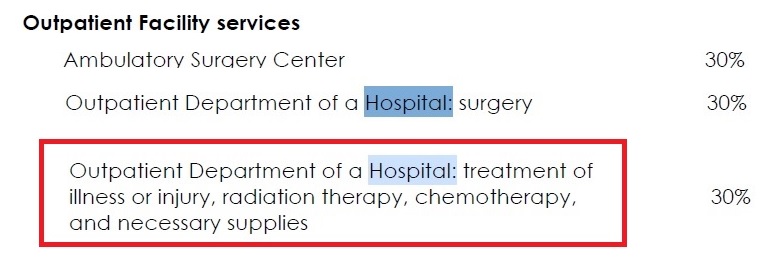
While the Bronze plans are fairly simple, the Silver plans can be a bit confusing. Health care services not subject to any medical deductible, means you go straight into the coinsurance percentage for outpatient procedures and durable medical equipment. In 2024, only the Silver 70 will have a medical deductible. This deductible must only be satisfied if you are hospitalized or in a skilled nursing facility. The Silver 70 and Silver 73 coinsurance for health care services is usually 30 percent.
Silver 73, 87, and 94 health plans, available through Covered California based on household income, have no medical deductible. That does not mean you escape any patient responsibility for health care services subject to coinsurance. With the enhanced Silver plans, you go straight into the coinsurance percentage for inpatient hospitalization and skilled nursing facility stays because there is no medical deductible.
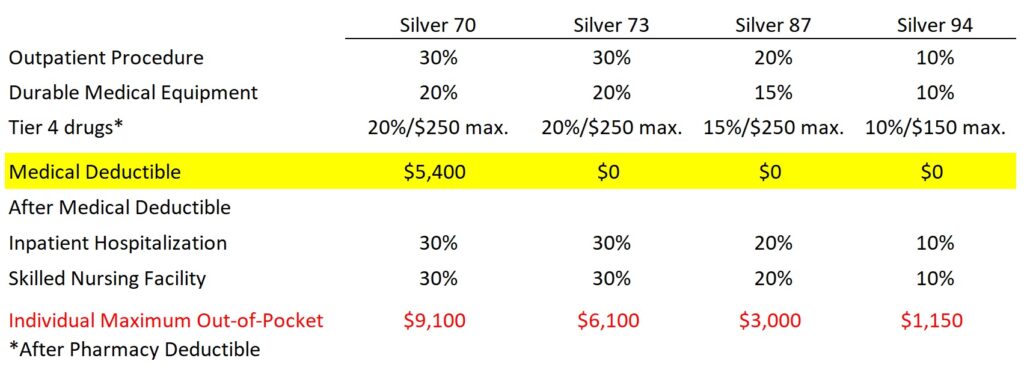
However, there will still be a cost to you, just minus any deductible the plans previously had. The coinsurance percentage for outpatient and inpatient health care services is 30, 20, and 10 percent for the Silver 73, 87, and 94 respectively.
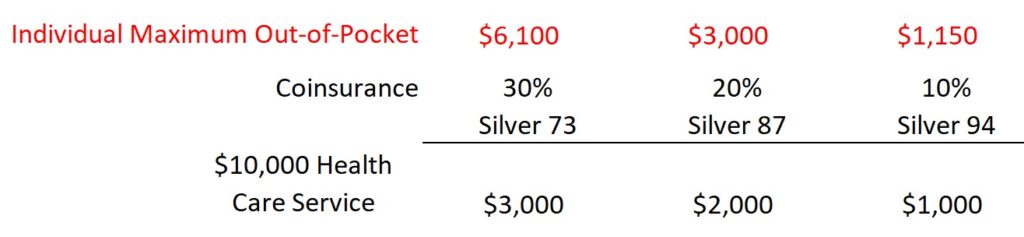
For example, if you had a medical procedure that generated $10,000 cost, under the Silver 73 you would be responsible for 30 percent or $3,000. The Silver 87 coinsurance responsibility would be $2,000 or 20 percent. Finally, under the Silver 94, you would be responsible for 10 percent or $1,000 of the health care service. Those large member responsibilities, by themselves, would not meet the maximum out-of-pocket amount for any of the plans.
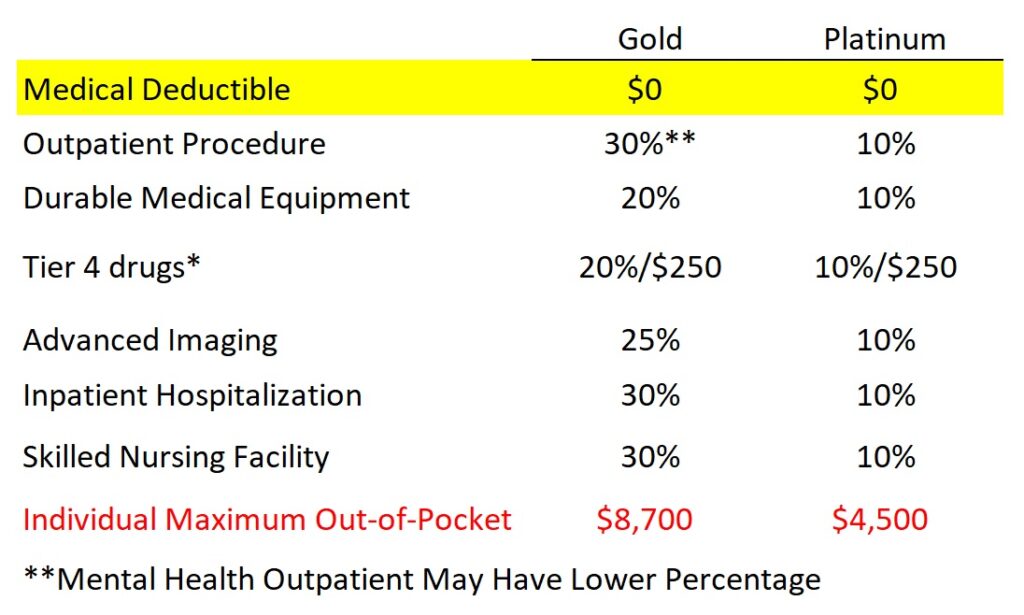
Gold and Platinum plans have no medical or pharmacy deductible. You go straight into coinsurance like the enhanced Silver plans. For the most part, Gold 80 will have a 30 percent coinsurance percentage. The percentage may be lower for some mental health services and advanced imaging procedures. Platinum has 10 percent coinsurance for outpatient and inpatient health care services.
There are times when a simple office visit at a set copayment results in an outpatient charge. This occurs when the doctor or nurse performs a therapeutic health care service. Perhaps you visit the doctor because your hearing is muted. The doctor diagnoses wax build up. The doctor or nurse cleans your ear and you can hear again. That wax removal may be billed as a service subject to your plan’s coinsurance.
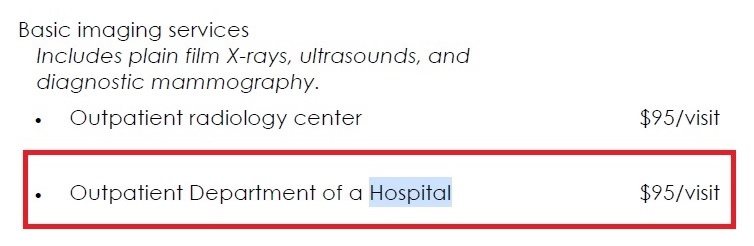
There have been reports that some plans may also bill a coinsurance percentage in addition to the office visit copayment because the provider is associated with the outpatient department of a hospital. This billing happens even if no therapeutic service is provided.
Unfortunately, we can not rely on the doctor’s office to inform us about potential costs. Some offices are better at informing patients of potential costs BEFORE the health care service. Do not assume that because the office did not tell you the facility was out-of-network, they are really in-network. There are many unexpected costs associated with health insurance plans that are never explained until AFTER they happen.
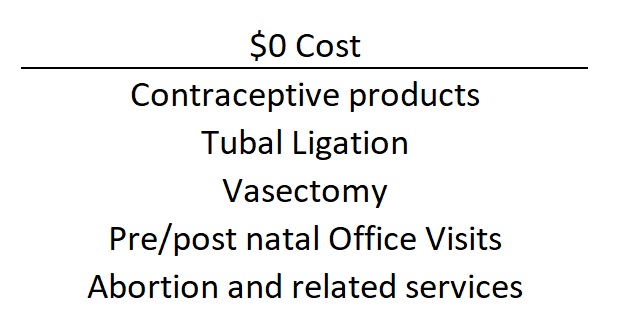
Vasectomies have been added to the list of no cost reproductive health care services in individual and family plans for 2024