One of the biggest questions I get is, “When will Covered California send me a bill for the health insurance?” Unfortunately, Covered California doesn’t invoice for the health insurance, that is left up to the insurance companies. If your application has been successfully transmitted to the insurance company you can make your first premium payment over the phone. Some applications have not, and may never, actually make it to your selected insurance company.
My health plan doesn’t have my application
Aside from many of the health plans having real problems mailing the first month’s premium notice to new applicants, many people have found that their chosen health insurance company never received the application from Covered California. I’ve called on several cases where the carrier has no record of ever receiving the enrollment application from Covered California. The carrier tells us to call Covered California and Covered California tells us to call the health plan. Now that the deadline for payment has past for some carriers, many individuals and families are now without insurance.
If you or someone you know is in this situation, let me know. I’m not trying to sell you anything. I just want to present to Covered California that their system has lost people. Perhaps if we get enough people come forward we can get Covered California to take this problem seriously.
Update July, 2014
It was confirmed from Covered California and one of the health plans that Covered California has been having IT issues with sending the enrollment data feed to the carriers since the beginning of July for health plans effective August 1st. Many carriers have either received no enrollment data or corrupted enrollment data. Either way, consumers who enrolled prior to July 15th are complaining that the carrier has not received their information and are unable to make their first binder payment to effectuate coverage. You can read more at August enrollments delayed through Covered California.
January 5th Update
- Covered California is sending out multiple emails to people to pay invoices, they have never received, by January 6th.
- Never send a payment to Covered California.
- Kaiser has been calling people and alerting them they have until Jan. 15th to make their initial premium payment.
- Many carriers have extended the payment deadline to January 10th such as Anthem Blue Cross.
- Never assume your payment date has been extended, call the carrier for a recorded message while you wait for an invoice.
Covered California releases payment information
Covered California released the following information to Certified Agents in an email about the first months premium payment. This was a good move because the staff at the Covered California call center were giving different answers to the same questions.
How will I get my premium bill and insurance cards?
Your health plan will send your first premium bill directly to you, as well as insurance cards once your premium is paid. We encourage you to pay as soon as you can once you receive your bill but no later than January 6th.
How can I pay my premium?
You need to pay the health plan you enrolled in. You can pay your premium bill by mail – but be sure you send it so the plan will receive your payment by January 6th. Your health plan may also accept payment through the phone or online, which will be faster than mailing your payment. Contact your health plan for more information about payment options.
What if I don’t enroll by December 23rd or pay by January 6th?
If you don’t enroll to have coverage start on January 1st, you can still get covered. Open enrollment extends through March 31, 2014, so you can still get coverage starting in February, March, April or May. See the chart below for upcoming deadlines and coverage start dates.
Avoiding a lapse in coverage
Many people are anxious to make the first premium payment so they will have no lapse in coverage between when their plan is cancelled on December 31 and the start of the new plan on January 1, 2014. Enrollments with premium assistance initiated in mid to late December may not get an invoice until after the New Year. Covered California has stated that those applications deemed eligible for premium assistance by December 23 will have retroactive coverage to January 1 even if the member receives and pays the bill later in January.
You applied, but where’s the bill?
If you are one of the thousands of households that mailed or fax in an application, along with some online enrollments, back in October or November and have received no invoice, it’s time to start making calls. You must start by calling the insurance carrier to see if they actually have the enrollment information. Some insurers have the applications but have not sent out bills.
It’s out of our hands
Even though you may have received a letter from Covered California requesting additional documents or discussing your 90 Day conditional approval, that doesn’t mean the insurance carrier has your information. I’ve called on several applications only to find the carrier has no information or bad information. Once Covered California transmits the enrollment data over to the carrier they no longer feel any responsibility to making sure the information they sent matches your application.
Blue Shield application deadlines
Blue Shield released the following information after being inundated with inquiries from consumers and agents.
IFP application deadline for January 1 effective date
Applications submitted through Covered California
Applications submitted through Covered California must be received by December 23, 2013 to be eligible for a January 1, 2014 effective date. Additionally, payment for the first month’s premium must be received no later than January 6, 2014.
Please note: If your client submitted a paper application in November, Covered California will process these applications by mid-December. Once processed, Blue Shield will send a request to your client for payment. Please encourage your clients to submit payment online for faster processing. Blue Shield will mail your clients’ ID cards about two weeks after the payment has been received.
Applications submitted through Blue Shield Applications submitted directly through Blue Shield must be received by December 15, 2013 along with first month’s premium to be eligible for a January 1, 2014 effective date.
Third Party Administrator
One tenacious client, not content to wait for an invoice tracked down the following information about making a payment over the phone for his Blue Shield health plan.
To pay online: https://service.healthplan.com/blueshieldca/binder Blue Shield had to have entered your data into their first premium payment system. Select Member Register link on the page. Enter the last 4 digits of your SS#, Birth Date and Zip Code. If you are in the system, you can create an account and pay online. If you are not in the system it will say no records found. That’s when you need to call Covered California to see if they have sent your information over to Blue Shield.
Health Plan Services (HPS), the nation’s leading technology, sales, retention and administrative services provider for the insurance and managed care markets, announced today that Blue Shield of California will utilize its Go-To-Exchange platform to streamline participation in the Covered California Exchange.
Included in the Go-To-Exchange platform are: ExchangeLink, a software platform that will be used to connect Blue Shield customers to Covered California, the state-sponsored public health exchange, and ServiceLink, which provides in-force administration, member billing, tax credit/subsidy collection, premium reconciliation and customer service. Blue Shield will leverage ServiceLink to ensure administrative functions are streamlined and high-quality customer service is provided to its members. “We are delighted to partner with Blue Shield of California through this initiative to ensure their members receive the highest quality service as they make critical health plan decisions,” said Jeff Bak, President and CEO of HPS. (The HPS number direct in Tampa is 877-300-9488.) The HPS direct number within Blue Shield is 877-755-4923. I wheedled it out of a regular CSR before she realized she wasn’t supposed to hand it out, or even acknowledge the existence of said department.
Blue Shield Binder Payment website, January, 2014
Blue Shield has added an online payment web portal through the above mentioned Health Plan Services provider. It will cross reference your personal information sent over from Covered California and allow you to make a payment to for your new health plan. Go to: https://service.healthplan.com/blueshieldca/binder. From the initial screen select Member Registration. Enter the personal information to see if your account pops up. If it does, you can then make a binder payment for your new health plan without waiting for the invoice. (click on the thumbnail image to enlarge)
If Covered California hasn’t sent your information to Blue Shield you won’t be able to apply any payments.
Calling early to confirm enrollment
Another client tripped across an access number for Anthem Blue Cross that will accept payments over the phone if they have the application on file.
FYI, in case any of your other clients need to contact BC about paying their premiums on new CC policies: When I called the number below, the rep directed me to call 1.800.333.0912 (this must be their unlisted number!)
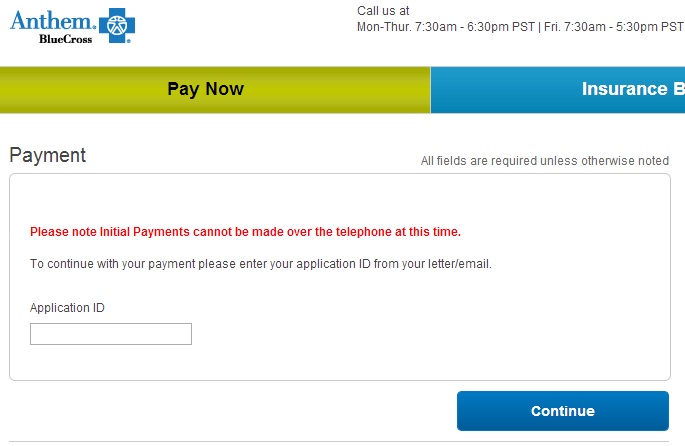
Anthem Blue Cross Payment Landing Page
Anthem Blue Cross Online Premium Payment
Thank you to a commentator who passed along the following information: If you are able to get your Application Control Number (ACN) or Application ID number you can visit the following url to make an online payment. https://shop.anthem.com/sales/eox/ABC/CA/en/payment/enroll/validate/landing?execution=e1s1
Did you really apply for health insurance?
Of course, as I’ve mentioned, the key is having your enrollment data successfully transmitted from Covered California to the carrier. If the carrier has no record or a corrupted enrollment file, and Covered California maintains it has been sent, all you can do is withdraw the application and start a new one.
Anthem Update December 30th
Correspondence from Anthem Blue Cross on Covered California payments –
Here is how the process is supposed to be working:
1. CoveredCA sends the application to Anthem Blue Cross
2. Anthem processes the application (taking around 5 days)
3. Once processed, Anthem mails out a letter with Initial Payment instructions and critical data to submit payment (ACN – application Control Number)
It is important for the applicant to wait for the letter to arrive as the letter has the vital information (ACN) needed to submit the payment and have the payment link to the applicant. Payments sent to Anthem without this vital (ACN) information run a high risk of being lost or not being able to be matched up with an application; potentially, leading to the applicant not receiving coverage for 01/01/2014.
It is to encouraged you wait, at least until Monday, January 6th for their letters to arrive in the mail. This will allow the system to work through its processes. If they have not received a letter by then, I would recommend them either calling one of these two Member Customer Service numbers: 855-634-3381 or 800-333-0912.
Additional Anthem Blue payment details, December 30th
The following is updated instructions on making the first premium payment for Anthem Blue Cross plans purchased through a state of federal exchange.
Details about initial payments for on-exchange plans
December 30, 2013
Initial payment notices are going out daily to your Anthem clients. Here is how the payment process works. Your client will receive a letter from us. This letter will explain what needs to be done to ensure proper payment gets made and that they are enrolled in their new health plan. The letter offers a variety of options for paying their first month’s premium, including bank draft, check, money order, eCheck or credit card. It also gives them a variety of ways to make their payment like:
- Signing into a secure payment page or
- Sending in a check or money order
The link to the online payment portal is listed below, but please advise your on-exchange clients to wait until they receive our letter about initial payment before making a payment on the portal. This will ensure a successful matchup of their payment and application. The payment portal doesn’t apply for your off-exchange clients who apply online, as the initial payment is part of the off-exchange online application process. If your client applied:
- For coverage ON EXCHANGE use this link.
Important note: A vital aspect to paying correctly on the payment portals is your client’s application ID, which can be found on the letter they will receive. The application ID is located on the top left hand side of the letter, underneath Applicant Name. If your client is interested in mailing in a PAPER CHECK, please advise them to include a copy of their letter with their check and to write the Application ID on the check or money order.
They can mail it to: Anthem Blue Cross P.O. Box 9041 Oxnard, CA 93031-9041
January 14th Anthem Update
Anthem Blue Cross extends payment deadline to January 31st.
From a client to who found the error and the solution: Anthem payment link is bad on Covered California website.
PROBLEM: As I told you yesterday, when I went to the Covered CA website, logged in and went to the Enrollment Summary page, I saw a Carrier Website address link for Blue Cross Anthem that was supposed to take you to the payment site. The link is: https://shop.anthem.com/sales/
SOLUTION: Today I figured out that the problem is that the Covered CA website link (https://shop.anthem.com/
See also Covered California paper applications threaten family insurance
Covered California drop health plan information
Insider information, pass it along
If you have the secret phone numbers for other health plans to allow Californians to make their first premium payments over the phone please post a comment with the information. We’re all surprised that it is this hard to actually send money to these darn insurance companies.
Kaiser Payments
Brian Higgins of San Diego passed along the following information regarding making payment on Kaiser health plans purchased through Covered California:
I found a Kaiser number that was at least slightly helpful: 866-799-3570. After about a 10 minute wait they confirmed info from Covered Cal is about 3 weeks behind but the payment due date has been extended to 1/10/14. They’ll accept payment by phone once the invoice is actually in hand. Called Anthem BC at 800-333-0912 and was told the due date has been extended to 1/10/14. Blue Shield at 877-755-4923 related that due date remains 1/6/14. They’re available until 8pmSaturday and 8am-6pm M-F.
Thank you Brian!
Can I go to my health care provider starting January 1st if I have not paid yet?
Covered California put out the following weak statement essentially encouraging you to beg you doctor to let you keep your appointment if you haven’t received and invoice for your health plan, paid the first months premium or even have a member ID number.
- Can I go to my health care provider starting January 1st if I have not paid yet?
As long as you pay by January 6th, you can use services covered by your health plan starting January 1st. First, be sure the provider (a doctor or other health service provider) is participating in the health insurance plan network you have selected. The provider may ask you to sign a statement agreeing to pay for the services if you cannot eventually prove you have health insurance. The provider may later send you a bill (“claim”) for the care. Once you have proof of health insurance coverage effective January 1, 2014, which you will receive after you pay for the insurance, you can submit the claim to your health plan to pay. It is also likely that by the time you get a bill or claim from your provider, you will already be entered into your health plan’s system. Simply call your provider and have them re-submit their bill directly to your health plan. Call your health plan to ask if the provider is in their network, if you have questions about whether a service is covered (included in your insurance plan) or about how to use your coverage. See the chart below for Covered California health plan contact information.
- How can I pay my premium bill for January coverage?
You need to pay your health plan — not Covered California – no later than January 6th. You can pay your premium bill (the bill for your health insurance) by mail, but be sure you send it so that your health plan will receive your payment by January 6th. Your health plan also might accept payment through the phone or online before you get your paper premium bill, which is faster than mailing your payment. Contact your health plan now for more information about payment options or if the January 6th due date is a problem for you. See the chart below for Covered California health plan contact information.
- When will I get membership ID cards for my health insurance plan?
Your health insurance company will mail you an enrollment package and membership ID cards within 10 business days of the health insurance company receiving your premium payment. You can still get care before you receive your ID card. But, be prepared for the provider to ask you to sign a statement that you agree to pay their claim if you do not later have proof of insurance. Once you have your ID card as proof of insurance, the provider can confirm your insurance and send the claim to the health plan.
Or…you can ask your doctor’s receptionist to call Covered California, wait on hold for 2 hours to talk to a call center staffer, and confirm that you indeed are signed up for a health plan.
Covered California Health Plan Payment Contact Numbers
[gview file=”https://insuremekevin.com/wp-content/uploads/2014/01/How_to_Make_a_Payment_CC.pdf” save=”1″]
[wpdm_package id=170]
Other Payment links