
Medi-Cal has taken over many of the functions of Covered California if any children are Medi-Cal eligible.
Several clients have contacted me regarding eligibility determination forms they have received from Medi-Cal, even though some or all of the family members have a Covered California plan with the tax credit subsidy. Even if the household information on the forms is wrong, Covered California consumers should supply the necessary information to their county Medi-Cal office or risk losing their private health plans altogether. Medi-Cal has effectively taken over the functions of Covered California if the family had been in Medi-Cal or if they still have children covered by Medi-Cal.
Medi-Cal Takes Over Covered California Functions
It has been a point of contention between Covered California and Medi-Cal for years that county Medi-Cal eligibility workers can supersede any determinations made by Covered California. Medi-Cal eligibility workers can make any changes they want to Covered California accounts without the consent of the consumer. For the 2017 open enrollment period, Covered California has announced that any consumer who has a Medi-Cal eligible child must report any changes to the household directly to Medi-Cal. Any changes to the household information through the Covered California account will be disregarded by Medi-Cal. This means any changes to income, household size, address, or anything else on the application for health insurance as entered into their Covered California accounts.
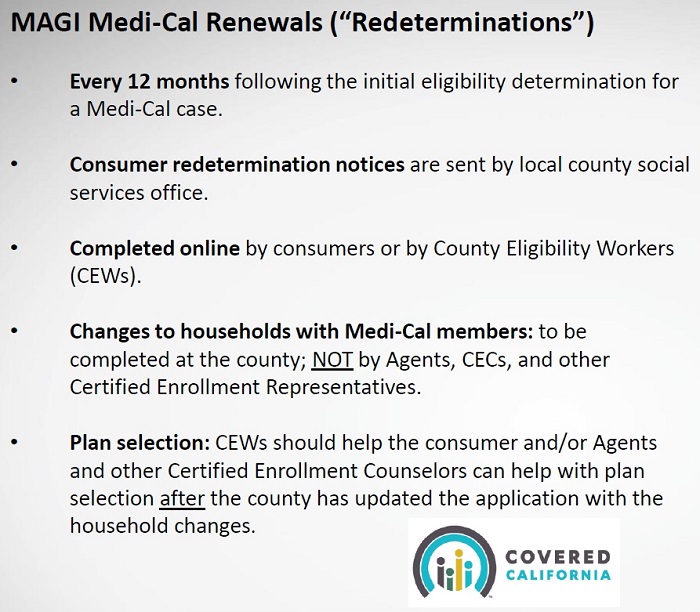
Medi-Cal has taken over essential function of Covered California. Covered California has instructed agents and CECs to refer families to their county Medi-Cal office.
Medi-Cal MC 216 Renewal Forms
Some Covered California consumers are getting confusing letters from their county Medi-Cal office. These Medi-Cal Renewal Forms (MC216) may not have all of the family members listed for re-determination. One woman received the renewal form even though she hasn’t been on Medi-Cal all year. This raises the issue of consumers being enrolled in both a Medi-Cal health plan and a Covered California plan with premium assistance. Is anyone auditing for these dual enrollments?

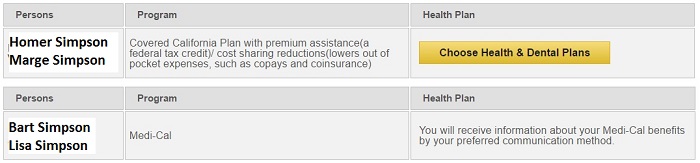
On November 1st, a county of Los Angeles eligibility worker changed the household income without approval or consent to do so. The whole family was then flipped into Medi-Cal.
If the forms are not filled out and returned, the individual or family runs the risk of being flipped back into Medi-Cal. If Medi-Cal doesn’t like the proof of income they unilaterally lower or erase the income altogether. This seems to have happened to one family who delayed sending in the Medi-Cal renewal form because they were under the assumption that everything had been handled through Covered California. The children were on Medi-Cal and the adults were receiving premium assistance for a private plan. In early November, a Los Angeles county eligibility worker reduced the family income and the adults were flipped into Medi-Cal. The first they learned of it was a letter from Covered California telling them their eligibility had changed.
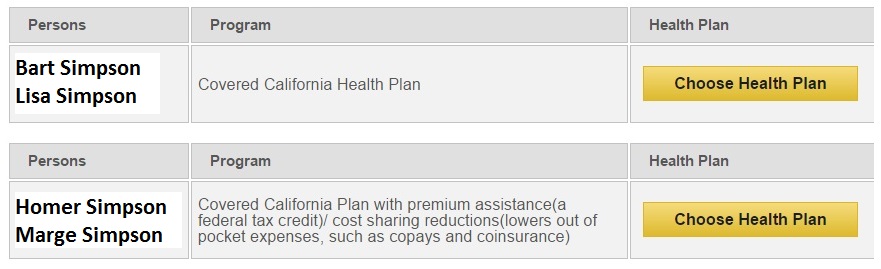
The Covered California system originally denied Medi-Cal to the children and denied them any subsidy to purchased a private plan. The family income was clearly within the range of adults with tax credits, children on Medi-Cal.
The Covered California enrollment system seems to be struggling to make eligibility determinations for children. The latest 2017 Covered California open enrollment online application is not always correctly determining when children are eligible for Medi-Cal. The odd eligibility determinations can sometimes be fixed with the Report a Change feature. But some children are showing their Medi-Cal being terminated at the end of the year.
After using the Report a Change function for this family, the children were finally determined eligible for Medi-Cal.
Essentially, the Covered California website is a useless tool for any household who has children in Medi-Cal. The must report all changes to the county Medi-Cal division. The whole point of Covered California was to make enrollment in health insurance easier for consumers. Because Medi-Cal has effectively taken over the functions of Covered California, Certified Agents, Certified Enrollment Counselors, and the Covered California staff themselves can provide little assistance for renewing health insurance for 2017. The net effect is that enrolling and renewing health insurance through Covered California is more difficult than it should be. The only people who seem have any control is a county eligibility worker that can’t be contacted.
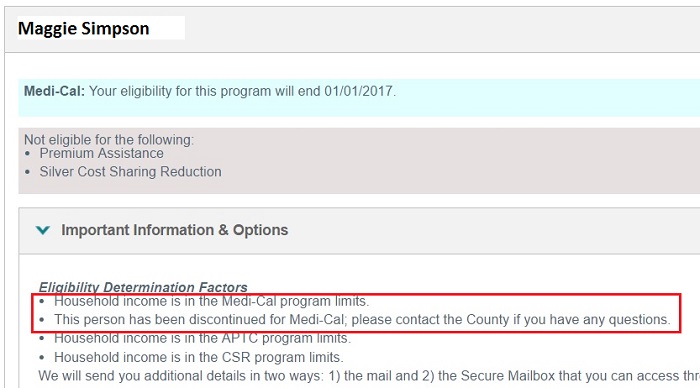
One family member was determined by the Covered California health plan renewal function to no longer be eligible for Medi-Cal. The Eligibility Determination Factors states the household income is in the Medi-Cal program limits.
[wpfilebase tag=file id=1926 /]


