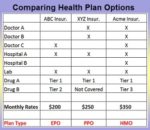
Of all the Medicare plans, the Part D Prescription (PDP) plans are the most confusing. The confusion arises because Medicare allows the Part D plans to offer alternate plans that differ from the standard plan. The alternate plans must be as good as the standard plan for the average Medicare beneficiary. Cost Sharing of the […]