Covered California Health Insurance Exchange
Covered California reviewed their proposed 2018 – 2019 budget at their May 2018 Board Meeting. Based on predictions from studies done by Pricewaterhouse Cooper (PwC) and the CalSIM team, the 2018 – 2019 fiscal year budget forecasts an enrollment decrease from 7% to 18% from FY 2017-18 and premium increases from 9% to 13%.
Lower Enrollment But Increased Revenue For Covered California in 2019
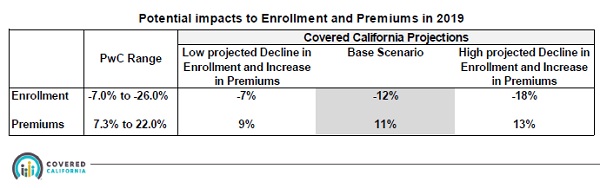
In 2019 Covered California predicts a decreased enrollment of 12% baseline scenario with at least a 9% increase in premiums.
Even though Covered California assumes declining enrollment in their health plans, because of the increased premiums they predict their gross revenues will increase anywhere from $12.4 to $27.9 million.
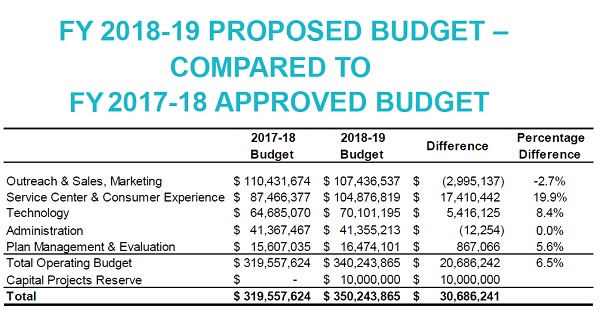
The proposed 2018-19 fiscal year Covered California predicts increased operating revenue over FY 2017-18 by 6.5%.
The increased revenue is also in light of reducing health plan assessment from 4% of the gross premiums down to 3.75% for the individual and family plan market. The proposed operating budget for FY 2018-19 is $340.2 million. This represents a 6.55 increase over the FY 2017-18 budget or an increase of $20,686,242.
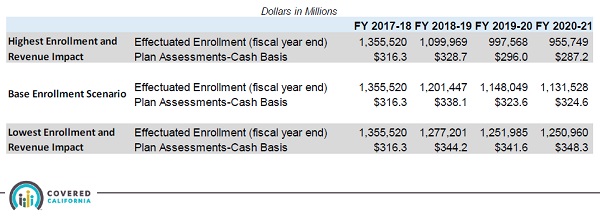
Even though enrollment is expected to decrease for FY 2018-19, the individual and family plan assessment revenue is expected to be larger than the previous fiscal year.
2018 – 19 Budget Adds Staff
The proposed budget includes
- Consumer Experience Division to measure consumer satisfaction and experience
- A new leadership academy for Covered California managers
- $107 million for marketing and outreach
- Adding staff to the Plan Management Division
- Funding a capital projects reserve of $10 million
- Covered California expects to have 1,399 positions in its organization supported by the proposed budget.
Agent Enrollment Is Largest Service Channel For Covered California
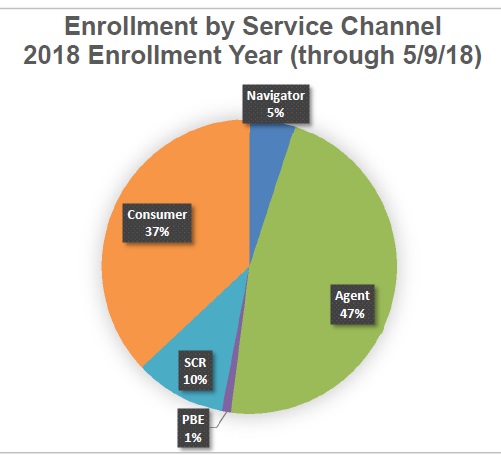
Previous to reviewing of the budget at their May meeting, Peter Lee’s Executive Director’s Report was given. Through early March 2018, 37% of enrollments were done by individual consumers, 47% of enrollments were entered by agents, and Navigators accounted for 5% of the enrollments.
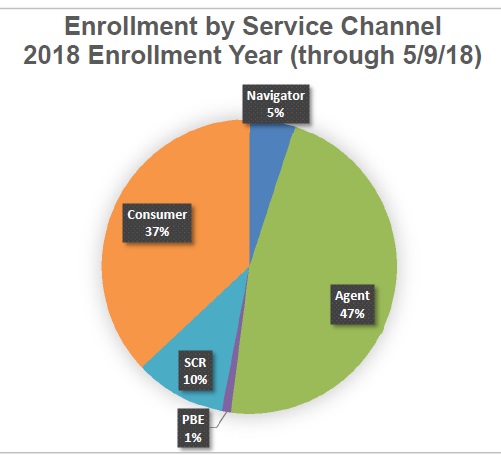
For the 2019 open enrollment period and SEP through May 9, agents enrolled 47% of consumers in health plans, 37% of consumers were self-service, and Navigators enrolled 5%.
There is a proposal to change how the Navigators are funded. Currently payments to Navigators are based on performance with possible adjustments in the next contract year. The new Performance Grant Model has payments based on reported performance by the grantee. The new model accounts for assistance to consumers where there might not be final enrollment.