In what has become routine for Covered California, they alerted agents to another CalHEERS enrollment website problem late on a Friday afternoon. The latest email notified agents that the system has been calculating the wrong Advance Premium Tax Credit (APTC) on submitted applications. While the Covered California email blast wasn’t real specific, it sounds like the APTC number is wrong when the applicant confirms the health plan purchase, but correct in the “Eligibility Results” page.
Covered California income error announcement
Dear Certified Agents,
An error occurred in the system this week that generates Advance Payments of Premium Tax Credit (APTC) amounts for the Individual Marketplace, resulting in applicants receiving incorrect APTC information.
The APTC allows federal tax credits to be applied to an insurance premium which lowers the overall premium cost for eligible participants. Receiving incorrect APTC information has resulted in some consumers obtaining an inaccurate estimate of their final premium costs.
The issue is expected to be resolved in the system fix this weekend; however, until the defect is resolved, you can visually verify that the correct APTC amount carries over to a plan selection by checking the “Eligibility Results” page. This is the correct amount of APTC that will apply to a consumer’s monthly premium. Agents can proceed with a plan selection on behalf of a consumer, but should ensure the consumer is informed of the correct APTC.
Covered California’s health plan carriers have been notified of the issue and are pending eligibility transactions until the issue is resolved. For consumers who have not yet selected a plan, they can continue with plan selection for an April 1st effective date and return to the website to confirm their APTC amount, again, anytime on or after this Sunday, March 16th.
System Maintenance
The system will be down from 10:00 pm Friday, March 14th until 6:00 am Saturday, March 15th for maintenance.
health plan carriers have been notified
Perhaps the scariest line in the whole email is, “Covered California’s health plan carriers have been notified of the issue and are pending eligibility transactions until the issue is resolved.” To me that sounds like they aren’t transmitting any enrollment data and a bunch of enrollments they have already submitted might be wrong. This could create another cascading log-jam of applications similar to the last week in December. Again, Covered California doesn’t give any hint as to the scale of the problem, we are left to guess.
More questions than answers
The email doesn’t say for how long the “error” occurred for or how many accounts it effected. We don’t know if the mathematical software issue impacted just new enrollments or current members making changes to their accounts as well. One result is for certain, the Covered California phone lines will continue to be swamped with a self-inflicted wound that Covered California hoped to hide with a late Friday announcement. Just when Covered California is making a final push before open enrollment closes, the website will be down Saturday morning.
Other math gremlins in the system
It might be sheer coincidence, but I was reviewing a client’s income that we had changed, and realized the Covered California system wasn’t
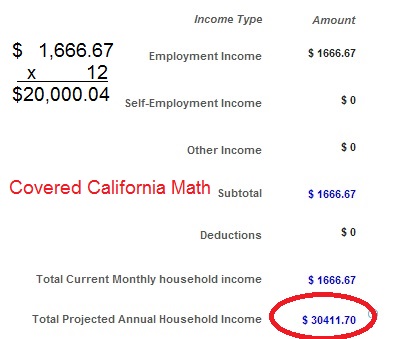
Covered California enrollment system can’t total household income properly.
totaling the monthly numbers correctly. It was so unbelievable that CalHEERS had ceased to perform simple math that I had to take a screen shot to send to my client. Two days later Covered California admits a problem with generating the correct APTC for accounts.
Constant Covered California website issues
The incorrect APTCs is just one of a never ending string of enrollment system issues and headaches for Covered California. Just last week it went down all day stopping enrollment in it’s tracks. But we never see the Executive Director Peter Lee or any of the Board members stand in front of the news cameras and apologize. They have become obsessed with “sales” and have made quality and service a low priority.