
Navigators complain it’s too hard to enroll people.
In response to Covered California Navigators complaints about not being able to fulfill their contractual obligations to enroll individuals and families in tax subsidized health plans the Covered California Board voted at their January 15, 2015, to advance grant money to Navigators just for talking to consumers.
The Navigator program was launch in the fall of 2014 by Covered California.
Covered California selected 66 organizations for funding, which includes an additional 161 subcontractors. Navigator Grants total $17.1 million, which includes $14.65 million in new Navigator funding and $3 million in roll over funding from the Outreach and Education Grant Program for the 18 Outreach and Education Grantees that are receiving Navigator grants. –Navigator Grant Funding Announcement Report.
Navigator enrollment goals
In order to receive the base grant funding level, each Navigator has to enroll a specific number of individuals into Qualified Health Plans through Covered California. Medi-Cal enrollments don’t count toward meeting the enrollment goals. The grant money is to be paid in 25% increments over the nine month grant period when the Navigator has reached 25% of the enrollment goal. For an enrollment to count the individual or family enrolled has to make their first month’s binder payment.
Navigators complain about consumers
Many of the non-profits that were awarded grants to enroll as few as 192 people began complaining that consumers were taking up their time asking questions. Navigators and the Certified Enrollment Counselors associated with them were providing lots of assistance on a variety of topics but not necessarily enrolling people into Covered California health plans. They lobbied Covered California to ease the conditions on which they were to be paid. Instead of being paid to enroll people, they wanted their grant money for talking to people.
Those darn Medi-Cal eligibles
Mary Watanabe presents Navigator complaints at Covered California Board meeting.
Mary Watanabe, Acting Deputy Director, Sales Division, presented the complaints and contract amendment to the Covered California Board. (Watanabe’s presentation starts at 1:39:50 of the Board meeting recording 9 or page 17 of the January 2015 Covered California Policy and Action Items that can be downloaded below). Among the complaints or challenges that Navigators were facing are-
- Providing substantially more assistance with activities that can’t be quantified, including renewals and explaining notices.
- An increased number of consumers who are enrolling online and calling the Navigators asking for assistance over the phone. The CEC provides the assistance and doesn’t get credit for the enrollment.
- Enrolling more people in Medi-Cal than was anticipated. Medi-Cal enrollments don’t count toward meeting their goal.
- Delay of receiving confirmation of actual enrollment by the family with is delaying progress payments.
Easing requirements for grant funding
The solution for relieving the Navigators from meeting enrollment goals, but receive the progress payments, is a change to the Navigator payment policy. The new policy, adopted by the Board includes –
- Count assisted applications through plan selection towards enrollment goals instead of effectuations. This change should allow many of the Grantees to be eligible for the next 25% payment.
- For organizations that do not meet 25% of enrollment goal; process the next payment upon satisfactory demonstration of their readiness and efforts to implement their campaign strategy.
Covered California in a state of learning
The often used excuse for approving the new payment policy was, “Covered California is a learning organization”. Covered California Executive Director Peter Lee said the payment policy change was necessary so the organizations could, “…front money to pay their staff”. To all the excuses for relaxing the contractual requirements of getting paid I say,
Welcome to the world that Certified Insurance Agents have been struggling with for the last year.
Consumer service isn’t easy
All of the complaints from the Navigators are shared by health insurance agents. Agents have spent innumerable amounts of time assisting consumers with renewals, notices, client’s getting busted into Medi-Cal, explaining MAGI, and now providing education on 1095-A. Agents routinely get calls from consumers for which they dutifully answer the consumer’s question only to learn the family is enrolling online and cutting the agent out of any commission for his or her assistance. And no one can predict when household members will be eligible for Medi-Cal until the application is submitted.
Glorified educators
The Navigator program is turning into an in-person certified educator program or extension of the call center staff. If the folks who developed the Navigator program would have just asked agents how much time they spend on customer support versus actual enrollments, they could have developed more realistic support and enrollment goals. The Navigators have witnessed the tough reality of sales. Just because you spend an hour helping someone doesn’t mean that person will ultimately purchase from you.
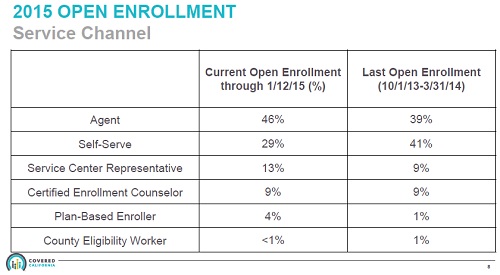
CECs under Navigators were only enrolling 9% of all individuals for 2015.
Navigator program not sustainable
While the intentions were good and it’s most likely having a positive impact reaching underserved populations, the Navigator program was not designed for sustainable operations. When these grants dry up, the assistance evaporates as well. Fortunately, the January 2015 Service Channel statistics shows Certified Enrollment Counselors only responsible for 9% of the enrollments for 2015 health plans. So when the Navigators close their doors there won’t be too many people looking for them to solve subsequent Covered California problems.
Navigator and Board files for download
- [wpfilebase tag=fileurl id=436 linktext=’Covered California Policy and Action Items, Navigators, 1-15-15′ /]
- [wpfilebase tag=browser id=71 /]
September 2014 post
Navigators to receive $190 per enrollment from Covered California
Covered California has award $17.1 million dollars to 66 organizations to be known as Navigators to enroll 93,467 individuals from October 2014 to June 2015. The average cost per enrollment for the Navigator program is $190 per person with some Navigators receiving as much as $435 per enrollment. For each additional 100 enrollments above the Navigator’s goal, they will receive an additional $7,500.
$17.1 million in Navigator funding
From the Executive Summary of the Navigator Grant Funding Announcement Report presented at the September Board meeting the highlights of the program were covered.
Executive Summary
On June 19, 2014, the California Health Benefit Exchange Board approved $16.9 million to distribute in grants to eligible entities through a competitive grant application process. A total of $14.65 million was allocated to provide grants to community organizations to reach an estimated 100,700 new Covered California subsidy eligible consumers. An additional $2.25 million was allocated for a bonus pool that is estimated to reach an additional 30,000 Covered California subsidy eligible consumers. Grantees who meet their enrollment goals would be eligible for a $7,500 bonus payment for each additional 100 effectuated enrollments.
Covered California selected 66 organizations for funding, which includes an additional 161 subcontractors. Navigator Grants total $17.1 million, which includes $14.65 million in new Navigator funding and $3 million in roll over funding from the Outreach and Education Grant Program for the 18 Outreach and Education Grantees that are receiving Navigator grants.
The 227 organizations selected to participate in the Navigator Program are estimated to enroll 93,467 individuals in Covered California Health Plans. The selected Grantees will reach consumers in 13 languages which include: Arabic, Armenian, Chinese, English, Farsi, Hmong, Khmer, Korean, Laotian, Russian, Spanish, Tagalog and Vietnamese. Many of the selected Grantees have proposed to provide services to multiple populations.
Medi-Cal enrollments not included
The Navigator Grant Funding Announcement, available for download at the end of the post, covered not only who received the awards, but the location, types of grantees, and the minority populations targeted. The Navigator enrollment goals are for Covered California tax subsidized health plans. Medi-Cal enrollments will not be counted toward meeting their goal. Consequently, we can expect Navigators to be aggressive in marketing to populations served by Certified Insurance Agents. Included in the Navigator awards is a certain portion of the funds to be used for marketing such as radio, TV, billboards and print media.
Recipients of the largest Navigator grants
| Grantee Organization | Award | Enrollment Goal | Cost per Enrollee |
| Clinica Sierra Vista | $500,000 | 3500 | $143 |
| Institute for Healthcare Advancement | $500,000 | 3200 | $156 |
| Kelly Rolfe Financial Services | $500,000 | 3500 | $143 |
| Koreatown Multipurpose Senior Center | $500,000 | 3500 | $143 |
| Redwood Community Clinic | $750,000 | 3000 | $250 |
| UHW | $500,000 | 3500 | $143 |
| Vision y Compromiso | $500,000 | 1150 | $435 |
Recipients of the smallest Navigator grants
| Grantee Organization | Award | Enrollment Goal | Cost per Enrollee |
| D’Access Central Inc. | $50,000 | 200 | $250 |
| Foothill Health Center | $50,000 | 300 | $167 |
| Greenville Rancheria | $50,000 | 192 | $260 |
| Physicians for National Health Program – California | $50,000 | 350 | $143 |
| Planned Parenthood of Orange and San Bernardino Counties | $50,000 | 350 | $143 |
Great marketing tool for associated products
Five tax preparation companies received $850,000 in grant money. The largest grant to a tax preparer went to Kelly Rolfe Financial Services. These companies will not only be paid to enroll people they will be able to market their other services and build name recognition along the way.
25% allowance for over-head
Covered California will allow the Navigator to spend the grant money within five different categories. There are specific maximum percentages for each expense category. If we apply the expense funding allocation to the total grant amount of $17,724,796 we get the following maximum expenditures for the total Navigator program.
| Expense Categories | Percentage | Total |
| Administration Allowance | 15% | $2,658,719 |
| Equipment Allowance | 10% | $1,772,480 |
| Outreach, Education, Media | 25% | $4,431,199 |
| Enrollment activities | 30% | $5,317,439 |
| Post Enrollment | 20% | $3,544,959 |
No MLR for Navigators
It’s interesting to note that the health plans must spend no more than 20% of their premium revenue on non-health care related services such as administration, profit, and marketing under the Medical Loss Ratios established by the ACA. Navigator will be able to spend 50% of their funds on non-enrollment activities.
Navigator oversight?
The presentation to the Covered California Board did not mention how the Navigators will be monitored beyond their enrollment goals. We don’t know if they go outside their target population and enroll individuals and families in another Navigator’s demographic if they will be penalized. Either way, look for lots of marketing during open enrollment from these Navigators and their contractors.


