Covered California will require verification of the Qualifying Life Event that makes a consumer eligible for a Special Enrollment Period.
Covered California has come under pointed criticism from the health insurance companies for their lack of verification of a consumer’s Qualifying Life Event (QLE) for a Special Enrollment Period (SEP). That will change as of August 1, 2016, when Covered California will start a program to randomly sample consumers who have enrolled in health plan outside of Open Enrollment under a QLE. Selected consumers will have to provide verification that they actually do have a QLE that makes them eligible to enroll outside of Open Enrollment such moving into California or the loss of minimum essential coverage like Medi-Cal or employer group coverage.
No proof Special Enrollment Periods
Many health insurance companies have cited that Covered California’s easy SEP enrollments has led to excessive claims being paid out by the health plans. In short, people without health insurance get sick and then jump into Covered California for health insurance in the middle of the year to get health care. But many of those consumers aren’t eligible for a SEP. They just want health insurance to pay for their medical bills. Premiums are kept low for everybody when the pool of health plan members includes the healthy as well as those who have health challenges.
Verifying Qualifying Life Events
The health plans have very strict guidelines for enrolling in health insurance directly with them outside of Open Enrollment under the Special Enrollment Periods. All the major health insurance companies require documentation of the QLE before the enrollment can be completed for their off-exchange plans. Some health plans have switched to only accepting paper applications, no online enrollments, for SEPs as an additional measure to filter out consumers who might be not really have a QLE.
Covered California verification process
Covered California has released a 2016 Special Enrollment Verification Tool Kit to help agents and certified enrollers comply with the new verifications.
Beginning August 1, 2016, consumers and enrollers completing an online application will be notified via updated language in the application that Covered California may seek to verify the validity of their self-attested Qualifying Life Event (QLE) in order to be eligible for a Special Enrollment Period (SEP). Review the 16.7 Release Notes for Certified Enrollers to review the change.
Covered California’s Office of Consumer Protection (OCP) will contact a random sample of consumers who enrolled during a SEP beginning August 1, 2016 to request proof of the QLE. If the consumer does not provide acceptable documentation of their QLE within 30 days of the date on the original notice, their coverage can be terminated.
If a consumer is found to have been fraudulently enrolled into Covered California without a Qualifying Life Event, the certified enroller who assisted the consumer could potentially lose their certification. Don’t risk losing your certification with Covered California and ensure all consumers who attest to having experienced a QLE are able to provide proof that they qualify for special enrollment.
The documents submitted to provide proof of the QLE will remain confidential and will only be used to determine eligibility for health insurance programs. They are not used for immigration enforcement purposes.
Consumers who enrolled in a Covered California health plan under a SEP, and are selected to provide verification or proof of their QLE, will receive Verification Request Notices in the mail. They will have 30 days to comply or their health insurance will be terminated. They will receive another notice if the verification they sent in is deemed unacceptable. Covered California has released a grid of Qualifying Life Events and the documents that are suitable to verify they are eligible for the SEP.
[wpfilebase tag=file id=1589 /]
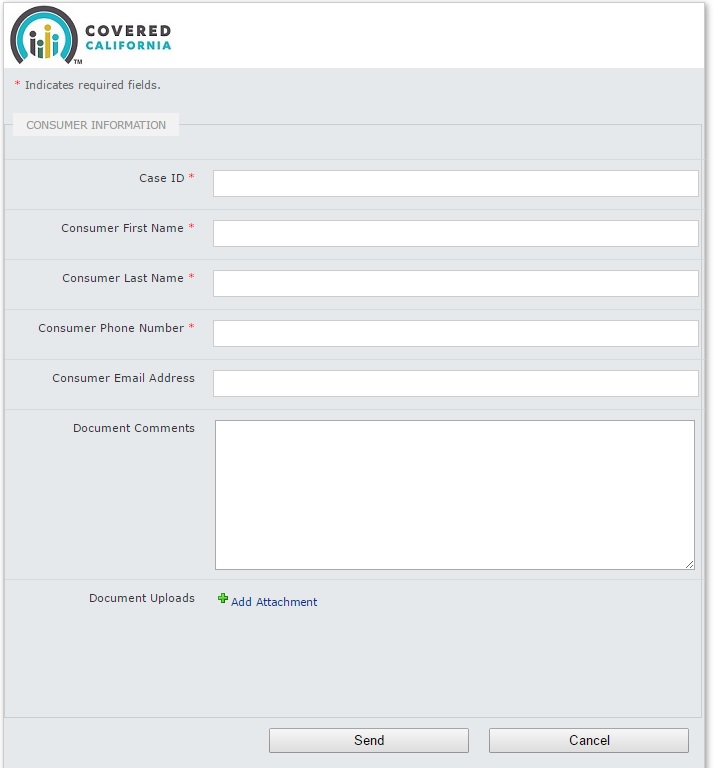
Special document upload site
Covered California has established a special web portal for uploading of the verification documents. It’s unclear why they did not add this functionality to the CalHEERS Covered California consumer account website that is already set up to accept verification for items such as proof of income and citizenship. Covered California will direct consumer, or their appointed agents, to use either an English or Spanish version of the QLE documentation website.
2016 Special Enrollment Quick Guide
Consumers who experience a Qualifying Life Event can enroll in a Covered California health insurance plan up to 60 days from the date of the event. This is called a Special Enrollment.
Certified Enrollers (Agents and Counselors) may assist all consumers eligible for a Special Enrollment. During this period, Certified Enrollers processing applications on behalf of a consumer will no longer have the ability to complete new or in progress applications without a Qualifying Life Event. New fields are displayed on the Application Signature Page that will require entry of a consumer’s Qualifying Life Event.
If applicable, consumers may choose from the following Qualifying Life Events. Eligibility and coverage start dates are determined by the type and date of the Qualifying Life Event.
| Qualifying Life Event | Effective Date |
| Birth or adoption | Day of birth/adoption |
| Lost or will soon lose health insurance | 1st of the following month |
| Marriage or Domestic Partnership | 1st of the following month |
| Release from incarceration | If plan is selected by the 15th, coveragage starts on the 1st of the following month. If plan selection is after the 15th, coverage starts on the 1st of the second following month. |
| Permanently move to California | |
| Gained citizenship/lawful presence | |
| Federally Recognized American Indian or Alaska Native | |
| Returned from active duty military service |
Consumers may also select “Other Qualifying Life Event”
- This selection should be used if the consumer’s life event is not listed, uncertain, or an exceptional circumstance and may require Covered California review of the application tovapprove the Special Enrollment
Consumers may also select “None of The Above (continue to review my application for Medi-Cal)”
- Special Enrollment does not apply to Medi-Cal applicants. These consumers can apply for coverage anytime during the year and do not need a Qualifying Life Event to gain coverage.
The consumer’s Qualifying Life Event date must be within 60 days to qualify for Special Enrollment. If the life event date is more than 60 days in the past, the consumer will not qualify for Special Enrollment.
2017 Special Enrollment Period Guide, Tool Kit, Accepted Documents
[wpfilebase tag=list id=396 pagenav=1 /]
2016 Files
[wpfilebase tag=file id=1593 /]
[wpfilebase tag=file id=1594 /]
[wpfilebase tag=file id=1595 /]
[wpfilebase tag=file id=1588 /]
[wpfilebase tag=file id=1590 /]
[wpfilebase tag=file id=1591 /]
[wpfilebase tag=file id=1592 /]
Covered California has not announced how many consumers will be required to verify their QLE each month for the SEP. There maybe additional glitches in the system as Covered California rolls out the new verification program. From experience, the health plans have been very strict on the documents that they will accept for the QLE. I have had them rejected because of incorrect dates on the letters from employers. The best advice is to have all the documents available to be uploaded if requested and apply as soon as possible for health insurance outside of open enrollment.