Covered California software issues of unauthorized dental enrollments, loss of subsidies from lack of consent for verification, over stated subsidy amounts to health plans, and duplicate active cases waste the consumer time and unwarranted stress.
After Covered California acknowledged at the January 2017 Board meeting that they had system issues that affected over 40,000 consumers, new enrollment problems seem to be boiling up. Some consumers have reported that household members who are ineligible for Covered California family dental plans have been automatically enrolled in dental insurance in 2017. In some very rare instances, the Covered California system is allowing consumers to actively enroll in two different subsidized health plans.
Ineligible Dental Plan Enrollments
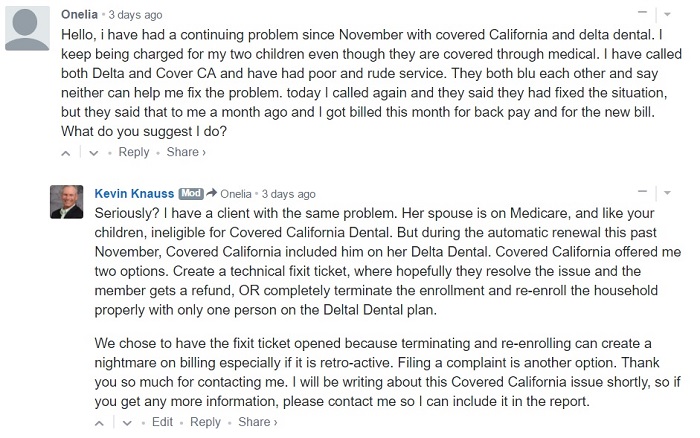
In December I had a client complain that she could not get Delta Dental to send her an invoice for her Covered California Delta Dental family dental plan. Delta Dental said they were having billing problems. We thought this was odd because like the health plan, the dental plan, was allowed to automatically renew for 2017. When the client finally got an invoice from Delta Dental it was for twice the normal amount. She called Delta Dental and was informed the Covered California added her husband onto her dental plan.
The only problem is that the client’s husband is ineligible for the Covered California family dental plan because he is on Medicare and not enrolled in a Covered California health plan. The requirement for enrolling in a Covered California family dental plan is that the household member is eligible for a Covered California health plan. The next challenge was how to fix the enrollment and remove the client’s husband.
Fixing Unauthorized Covered California Family Dental Plan Enrollments
Covered California dental and health plans will only make changes to enrollment when they come from Covered California. You can’t call the dental or health plan and either add or remove a child or spouse. All changes must go through Covered California. In order for my client to have her husband removed from the dental plan retroactively and so she could get the premium amount she paid for her husband returned to her (she had to pay the full amount to keep her dental plan active), we had to have Covered California fix the problem. When I presented the problem to Covered California they offered me two options to dis-enrolling the ineligible household member.
- Terminate both the health and dental plan as of January 1, 2017 and re-enroll just the eligible household member in the same health and dental plan without the spouse on the dental coverage.
- Create a Trouble Ticket to fix the error internally.
I chose the Covered California Trouble Ticket option because I’ve experienced major issues when Covered California terminates coverage and re-enrolls a household. Usually, the health plan only gets the termination and never the re-enrollment information leading to parents crying on the phone because their children no longer have health insurance.
Covered California Software Glitches
While no one at Covered California indicated that this unauthorized dental enrollment raised a red flag, to me it signaled another software failure like had happened earlier in the year to 40,000 other members. (See How To Cope With Covered California Glitches by Emily Bazaar.) I also did not know if my client was just a one-time random software failure occurrence. Then a woman left a comment on my blog post about filing a complaint with Covered California. This consumer had her Medi-Cal eligible children enrolled on her Delta Dental family plan. Children in Medi-Cal are ineligible for a Covered California family dental plan because they can’t be enrolled in a Covered California health plan.
I don’t know how widespread the problems of unauthorized dental plan renewal enrollments are. I’m not sure if it is limited to just Delta Dental or if it is occurring with other dental plans. While Covered California alerted agents and consumers about their earlier software errors, they provide no information regarding the specifics. In other words, did the system errors have any common denominators such as zip codes, regions, health plan types, mixes households, etc. But another quirky enrollment situation I ran into were clients enrolled twice with Covered California health plans.
Duplicate Active Covered California Enrollments
In January I was contacted by a woman who wanted my assistance with changing her current Kaiser health plan through Covered California to a different plan that would support a doctor she wanted to see. She designated me her agent in her Covered California account, but when I looked at the enrollment history, there was no Kaiser health plan listed. I was not necessarily surprised at the lack of prior or current enrollment because people can have duplicate accounts that are inactive. It was also possible that her Kaiser plan was really an off-exchange plan and not through Covered California.
After we enrolled her family into a Chinese Community Health Plan starting March 1st, she asked me to terminate her Kaiser plan. But I had no record of current enrollment. Fortunately, she had received her 1095-A form listing her OTHER Covered California case number. I called Covered California and they confirmed that the primary applicant with the exact same social security number was enrolled with two different health plans, under two different case numbers and was eligible for Advance Premium Tax Credits (APTC).
Two Cases Both Eligible for Monthly Tax Credit Subsidy
Right on the cusp of the first double-case enrollment, I had another client ask why he was receiving Oscar Health Plan invoices when I had enrolled him in a Blue Shield plan back in December. Similar to the first situation, this gentleman had two different case numbers and was approved for the APTC from Covered California. I verified the dual enrollment with Covered California by my client’s social security number. Again, I had to tell my client he had to cancel one of the plans. He could not receive the tax credit subsidy for both plans. While the gentleman remembers talking to an Oscar Health Plan agent on the phone, he didn’t remember authorizing enrollment.
Under no situation should an individual, especially the primary applicant, with a unique social security number, be determined eligible for APTC under two different case numbers. The system should catch potential duplicate subsidized enrollments and prevent them. I’m not as worried about fraud as generating a nightmare 1095-A scenario for the consumer. I completely understand that some people transition from one household plan to another because of divorce, marriage, or age and could inadvertently have two subsidize health plans in force for a small amount of time.
The accumulation of duplicate tax credits for even one or two months can create a nightmare tax reporting scenario. With a system as complicated as Covered California this is bound to happen. But the system should not let a primary applicant, who is the primary tax filer, have two different active cases where they are eligible for the APTC.
System Checks To Prevent Mistakes
Covered California does have some built-in checks to help consumers and agents navigate the system. It has been my experience that if a family, whose children are already in Medi-Cal, attempts a Covered California enrollment, Covered California will cross reference social security numbers to prevent dependents from being enrolled into a subsidized plan until they have been released from Medi-Cal. This is also the case for adults who may be on Medi-Cal and attempt to enroll in a subsidized health plan through Covered California. There are also numerous pop-up windows to notify consumers when they are about to make selection that might not be in their best interest such as when removing a household member from the family plan.
If there ever was an alert or notification that a primary applicant had another active account where they were receiving the APTC, I have not seen it. In the two cases with duplicated accounts that I am aware of, each of the consumers had worked with either a certified enroller or agent they could no longer contact. This is a real weak link when it comes to providing customer service. Individuals and families may enroll at an event sponsored by a health plan or Covered California store front, but the agent or certified enroller is nowhere to be found if a problem occurs with that enrollment.
No Concern For Duplicate Enrollments
Folks at Covered California dismiss this overlapping scenario based on their assumption that a consumer would never pay two different health plan premiums. First, the CalHEERS Covered California application system cannot make assumptions of personal behavior. The system should be designed to prevent duplicate enrollments or at least notify the consumer or agent that one exists. Second, Covered California should not assume people won’t make two different health plan premiums when both are being subsidized. There are people who will have two health plans to make sure all of their doctors are in-network. For some people, paying two subsidized premiums is cheaper than paying the out-of-network costs for some health plans.
Finally, Covered California doesn’t understand what consumers go through when it comes to dealing with health insurance companies and filing taxes. Some of these health plans are relentless when it comes to sending letters demanding payment for past premiums when the member has already enrolled in a different plan. It verges on harassment and causes significant stress for some consumers. When it comes to federal taxes, completing Form 8962 Premium Tax Credit reconciliation can be very daunting. When a tax payer receives multiples of 1095-A, B, or C, the confusion of sorting out the mess can be horrendous. I’ve been told that ultimately, the Covered California system would catch duplicate subsidized enrollments. I believe them, but it should not be allowed to happen in the first place.
For Covered California, there seems to be little concern about a consumer’s travails in sorting health plan problems. Their attitude is that their responsibility stops with enrollment. Their empathy only extends to what they can control. If their system or erroneous advice causes unmitigated anguish for consumers, they seem not to be overly concerned. Even Peter Lee, addressing the issue of errors that resulted in over 20,000 consumers either being offered APTC without proper consent for verification or the 25,000 consumers having an overstated APTC amount being sent to their health plan, was not centered on the challenges his customers faced, but with the Covered California brand. He commented at the January Board meeting, “Again, the total of these numbers is less than 3% of our enrollment.” Peter Lee went on to admonished the media (those who would write about the glitches) that these billing issues should be compared to the other small percentages of consumers who have problems with their phone bills. (See: January 26th Covered California Board Meeting Recording, Time Mark 16:20.)
Peter Lee’s statement’s epitomizes a lack of connection to the consumer experience exhibited by large government agencies. Phone and utility companies routinely have billing problems. Only having 3% of your consumers affected, when you are servicing 1 million, is a small number. But a phone bill is different from health insurance. You won’t die if your mobile phone is disconnected. You can die if your health insurance is cancelled. And the phone company usually apologizes profusely when they have caused widespread customer inconvenience because of billing errors.
Similarly, having unauthorized household members enrolled in a family dental plan or allowing a consumer to receive APTC for two different health plans, will cause the consumer wasted time at the very minimum to rectify the situation. The worst case scenario is a protracted battle with the dental and health plans to refund premiums and another headache when it comes to wrestling with taxes. But none of these consumer issues are viewed by Covered California as problems that they should be concerned about.