Covered California has issued an alert that during this period of coronavirus covid-19 economic slowdown, many consumers are changing their incomes and getting snagged with Medi-Cal eligibility. While there is nothing wrong with Medi-Cal if you are eligible, incorrect income changes can result in a Medi-Cal eligibility determination and it can be frightfully difficult to untangle the knot.
Medi-Cal Carry-Forward Status From Covered California
How to help consumers who have been found Medi-Cal eligible after incorrectly entering their income
On March 16, the Department of Health Care Services (DHCS) directed counties to delay discontinuances and negative actions for Medi-Cal beneficiaries for 90 days due to the Coronavirus (COVID-19) pandemic. On April 10, the DHCS issued another information letter to clarify that counties may process voluntary discontinuances if consumers request them. Consumers who were moved into the Medi-Cal income threshold by mistake (i.e., because they reported incorrect income) must update their case after their voluntary discontinuance is processed in order to return to Covered California enrollment and be evaluated for financial assistance eligibility.
Please see two sample scenarios and next steps below for a current Covered California consumer who incorrectly reported their income, entering a number within the Medi-Cal limits, and was found eligible to Medi-Cal:
If the consumer’s case has been placed into Carry-Forward status and the County has not begun processing the referral*, the consumer or their delegated enroller can update the application within CalHEERS to correct the entered income and remove the consumer’s Medi-Cal eligibility. Enrollers can identify cases in Carry-Forward status by the multiple program eligibilities that show in the Household Eligibility Results Summary page of the application:
Eligibility results will show Covered California, Premium Assistance, AND Medi-Cal.
*Note: Since the county will have received the referral, they may still attempt to process the referral at a later date even after the consumer’s income is corrected within the application. If the consumer receives a request from their county for information, they should comply with the county request or request voluntary discontinuance at that time. If they do not, the income correction made in the application may be reverted by the county, placing the consumer back into the Medi-Cal income threshold.
If the consumer’s case has already transferred to the county, further action is required:
- The consumer must contact their county to request a voluntary discontinuance.
- The county will process the voluntary discontinuance request.
- The system will end-date the consumer’s Medi-Cal eligibility and re-run eligibility**. (The consumer’s income will still show as within Medi-Cal limits, so the system will determine the consumer not eligible to financial help through Covered California.)
- The consumer must log into their portal to report a change, now correctly reporting their income.
- The consumer will be found eligible to Covered California programs. (If the consumer’s corrected income makes them eligible to financial help through Covered California, that financial help eligibility will now show.)
**Note: These changes would be moving forward, meaning that if a consumer was deemed Medi-Cal eligible, even in error, correcting the application and restoring eligibility for Covered California would be prospective (for a future effective date) only.
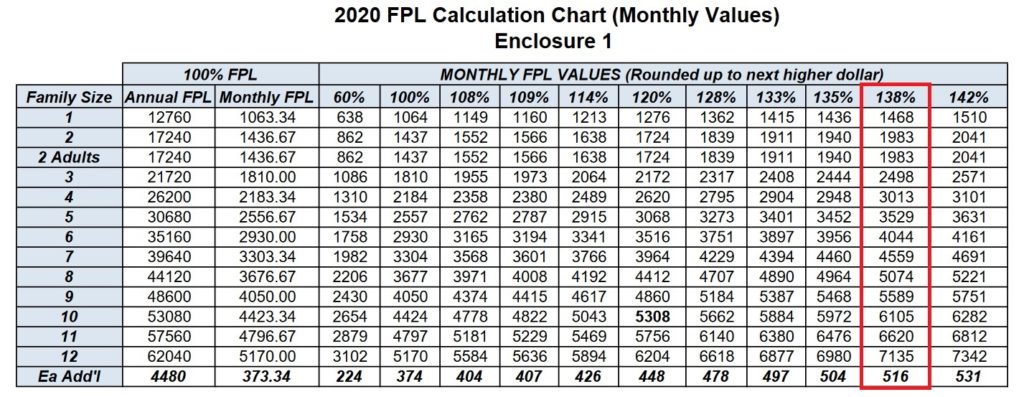
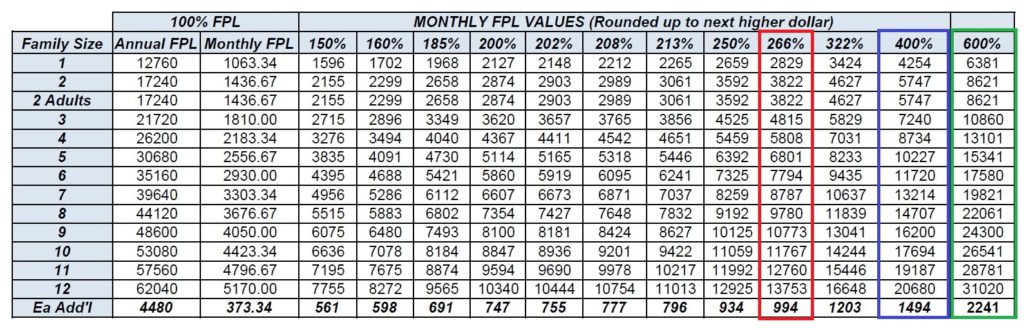
Covered California screens for Medi-Cal eligibility based on your monthly income, not annual income. Therefore, it is imperative, that when you are reporting a change to your income that the monthly income be accurate relative to published 138% of federal poverty level for adults and 266% for children.
The error that typically occurs is changing an existing income entry down to zero for the year (because you no longer have the job) or putting in the wrong end date. Another issue is not starting the new unemployment compensation with the correct date. The income section is very date sensitive. Always check your MONTHLY income estimate on your Covered California account BEFORE you proceed and submit the application or report a change submission.
If your changes result in a monthly income below the Medi-Cal threshold, you will be determined eligible for Medi-Cal. The system is screening for Medi-Cal in the month of the change or application. It does not consider future income amounts. If you make a change in May, resulting in low or no income for May, but your new income starts June 1 – and maybe too high for Medi-Cal – you will still trigger a Medi-Cal carry-forward status because the month of the application or change report has a low income amount.