As Medi-Cal returns to normal operations for determining eligibility for a variety of programs, here are a few tips to keep Medi-Cal or transition to Covered California.

Tips For Renewing and Updating Medi-Cal Enrollment
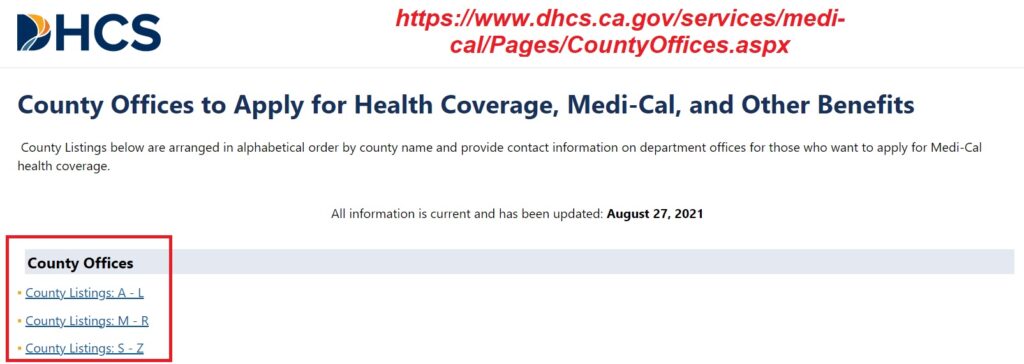
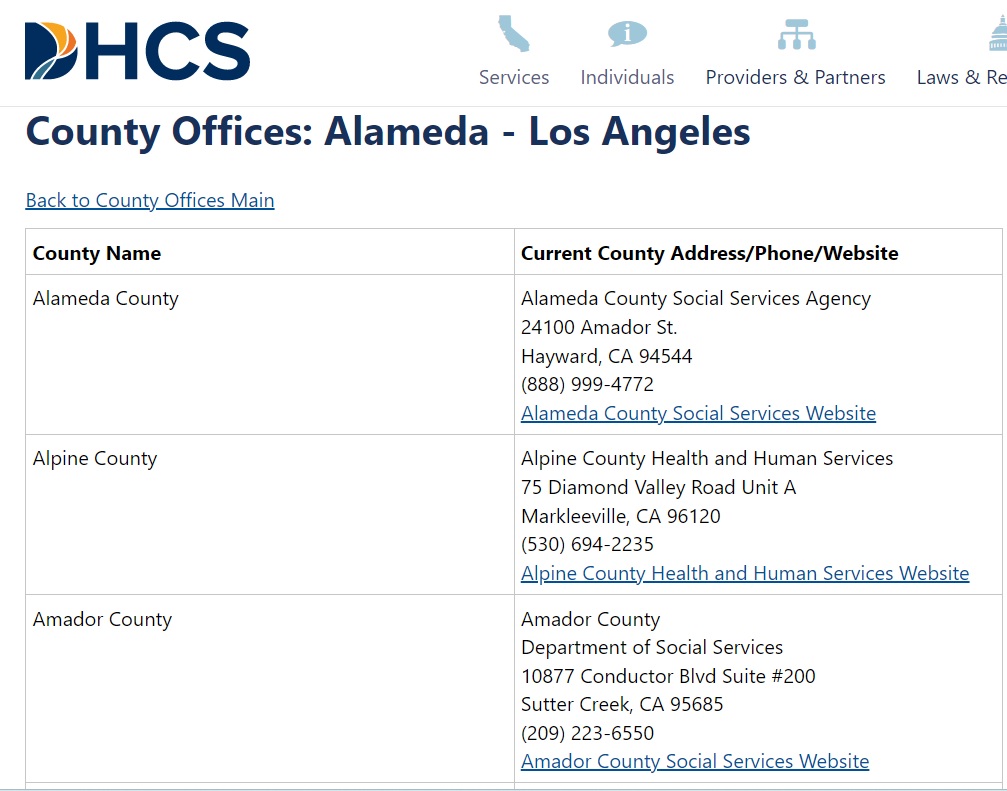
Each county handles Medi-Cal eligibility and enrollment. The California Department of Health Care Services manages the Medi-Cal programs. You need to be in communication with your county Medi-Cal office to update information in the Medi-Cal system. To find your county office address, phone number, and website visit https://www.dhcs.ca.gov/services/medi-cal/Pages/CountyOffices.aspx
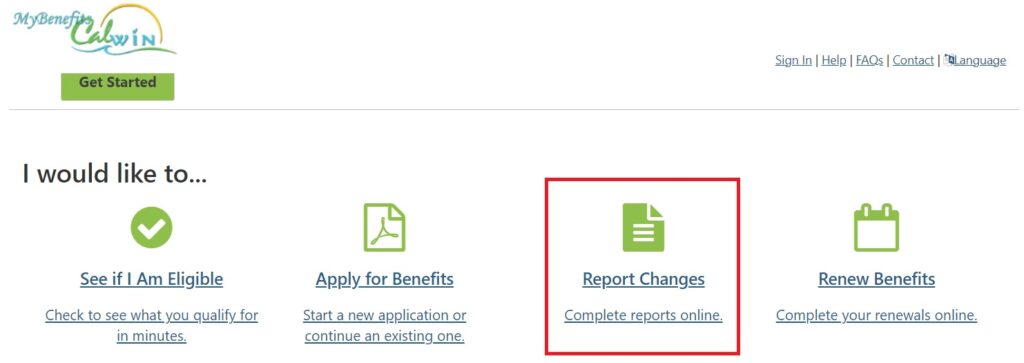
It is important to keep your contact information and address current with your county Medi-Cal office. The best way to do this is to create an account with one of the beneficiary portals. The portal you use is based on your county. There is BenefitsCal and MyBenefitsCalWin. Below is the list of counties and which portal application they use.
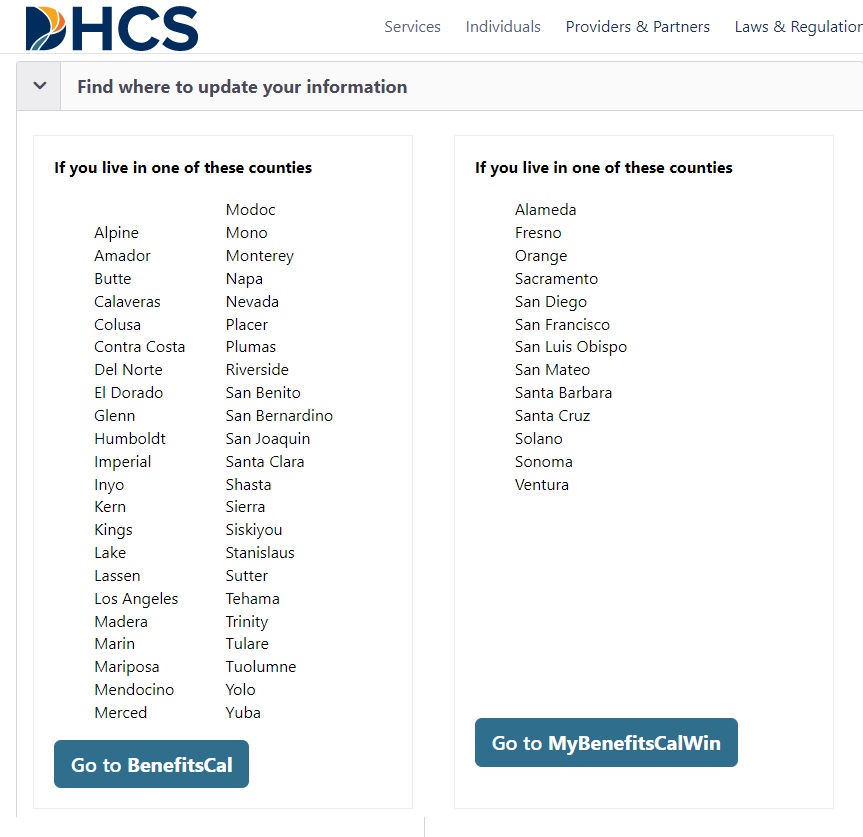
From the portals you can upload documents and report changes such as a change of address.
Annual Redetermination Medi-Cal Forms
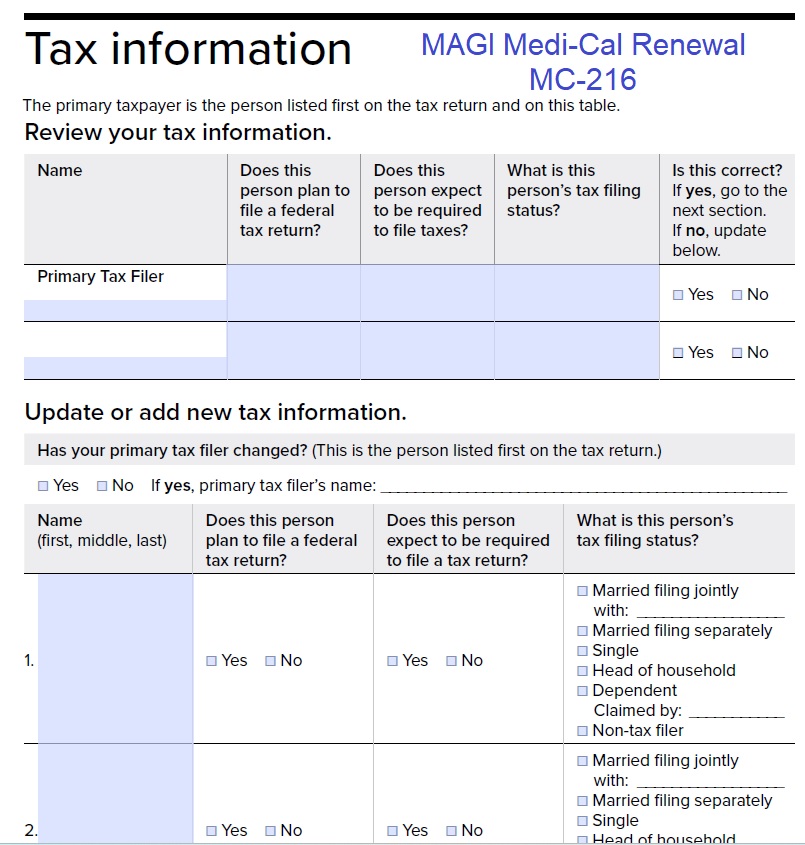
Medi-Cal must send paper forms and notices. If you are enrolled in MAGI Medi-Cal, you will receive renewal form MC-216. MAGI Medi-Cal, like Covered California, is based on the tax household and a primary tax filer must be listed.
Non-MAGI Medi-Cal beneficiaries will receive renewal form MC-210. This form of Medi-Cal is conditioned upon income and assets. MAGI Medi-Cal only looks at the household income, not your assets. You may receive the Non-MAGI Medi-Cal renewal form that may seem like a mistake. However, some families have household members in different types Medi-Cal programs. There may be family members with MAGI Medi-Cal and other family members in Non-MAGI programs.
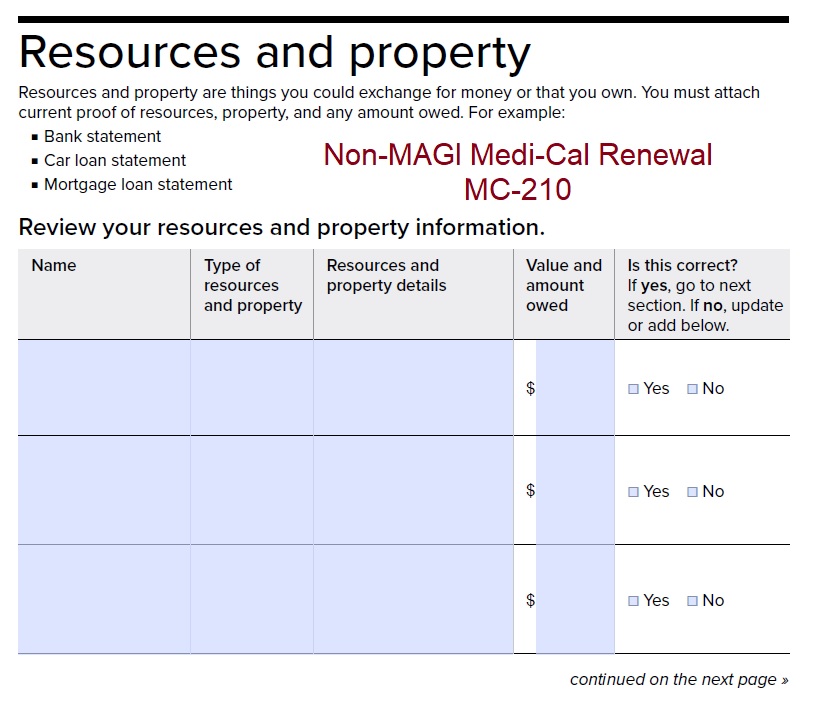
Fill out the form to the best of your ability from documents related to the assets. Because the asset limits will be removed for 2024, Medi-Cal has noticed that they have been given a waiver from the federal government not to scrutinize assets of current Non-MAGI Medi-Cal beneficiaries for certain programs through the end of 2023.
You will receive a notice of action as to whether you are still Medi-Cal eligible or no longer eligible. If you do not agree with the eligibility determination, you can appeal the decision and provide more information about your situation.

Medi-Cal to Covered California Auto Enrollment
MAGI Medi-Cal individuals who are terminated because their incomes are too high to qualify will be transitioned to Covered California. This is all to avoid a gap in coverage. You do not have to accept the Covered California enrollment with the subsidies. If you have an employer sponsored health plan, you may not be eligible for the subsidies. To read more about the transition, go to Automatic Enrollment into a Covered California Silver Plan When MAGI Medi-Cal is Terminated.
You may not have informed your county Medi-Cal office of your higher income or that you now have employer sponsored health insurance. You can report that information through the beneficiary portals. It may also be captured when you fill out the renewal forms. Either way, you won’t be liable for the costs of Medi-Cal health insurance and services. It is just important to report the new household information so Medi-Cal can properly terminate your enrollment. You can read more at Do I Have To Repay California Medi-Cal?


