County Medi-Cal departments have resumed normal operations after the Covid Public Health Emergency has ended and it is anticipated that thousands of people will have their MAGI Medi-Cal enrollments terminated. California has devised process to help individuals, families, and children to be covered with health insurance if they no longer qualify for MAGI Medi-Cal with an automatic plan selection at Covered California.

There are a variety of reasons why your MAGI Medi-Cal enrollment is terminated from a lack of response to the annual redetermination paperwork to your increased income. However, once your county Medi-Cal office determines that they you are no longer eligible for MAGI Medi-Cal you will be sent a series of letters IF the county has your current address. The information outlines the process of moving from MAGI Medi-Cal to Covered California health plan with the subsidies.
Flow Chart of Medi-Cal to Covered California Automatic Plan Selection
The Automatic Plan Selection process of offering a Covered California health plan for terminated Medi-Cal beneficiaries is complex. Instead of granular details, that are listed in official letters, I present a flow chart of the process.
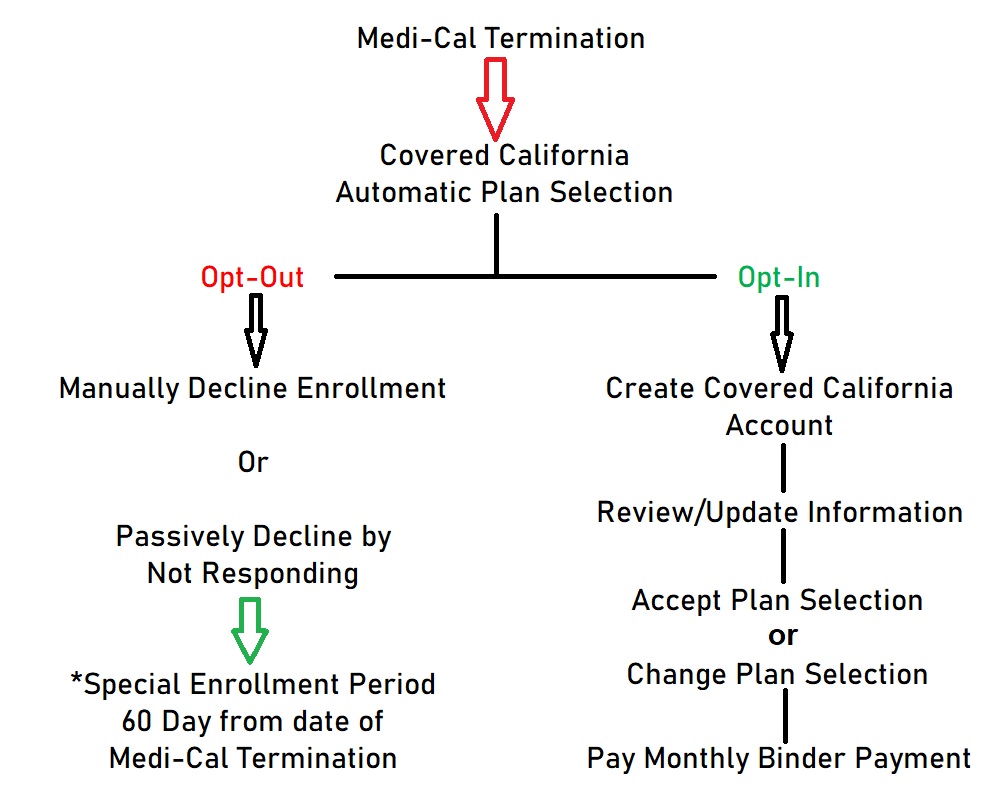
When Medi-Cal enrollment is terminated for you or your children, they send the information to Covered California. In addition to letters from Medi-Cal, Covered California will also mail letters outlining the Automatic Plan Selection Process.
You can opt-out of the Covered California enrollment. You may have moved out of state or gained other coverage such as employer sponsored health insurance or Medicare. You can visit the special Covered California website for the Automatic Plan Selection and opt-out. You can also passively decline by not responding and letter the initial enrollment lapse. However, with the termination of Medi-Cal you have a 60 day Special Enrollment Period to enroll in a Covered California plan, employer sponsored plan, or into an off-exchange health plan direct from the carrier.
If you decide to opt-in to the Automatic Plan Selection process, you will be prompted to create an account if you don’t already have a Covered California account. Once the account is created you can review the information Covered California has received from Medi-Cal and make any updates. For example, you may have moved since the time of the original Medi-Cal enrollment. You will want to update the address so the proper health plans, rates, and subsidies can be calculated for the new address.
After updating your information you can review the health plan you or your family members have been enrolled into. At this point you can change the plan selection. To complete the enrollment you need to accept the terms and conditions of enrollment into Covered California and pay the first month’s premium, also known as the binder payment. Some plans may have a $0 premium because the subsidy is equal to or greater than the plan premium. Regardless, you still have to accept the plan selection and agree to the terms and conditions of enrollment.
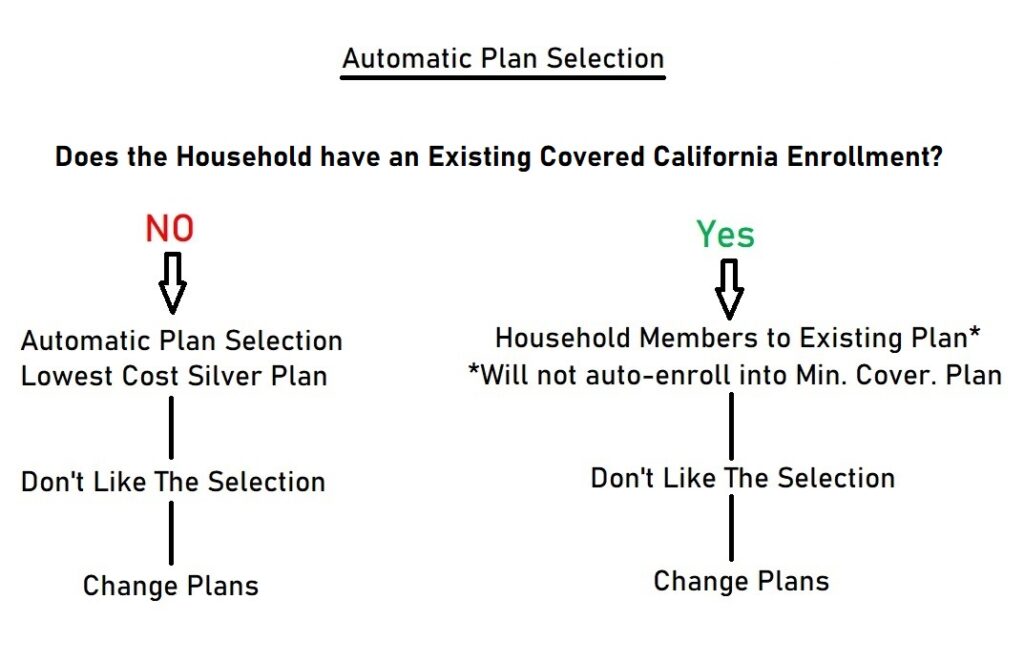
How is the Automatic Plan Selection Determined?
If there is no existing enrollment of any family member into a Covered California health plan, the default plan selection in most cases will be the lowest cost Silver plan. For many people with low incomes, there may be no monthly premium for the lowest cost Silver plan. If you don’t like the plan selection, you can change it. For example, you may have been enrolled into a Kaiser Silver plan, but Kaiser is not convenient for you. You can select a different Silver plan carrier offered in your area. You can also select a Bronze, Gold, or Platinum plan. Just remember that there a higher benefit health plan like a Gold or Platinum will usually have a monthly premium associated with it.
If there is an existing Covered California enrollment, in most situations, the terminated Medi-Cal household members will be grouped with the existing enrollment. For example, your children are no longer eligible for Medi-Cal and you have an Anthem Blue Cross Gold plan. Covered California will include them on your Gold plan. Of course, you can change their enrollment to a different carrier and metal if you want. However, household members will not be enrolled in a Minimum Coverage plan, it would default to the lowest cost Silver plan.
You can always delegate a Covered California Certified Insurance Agent to navigate the Automatic Plan Selection process. It can be complicated and complex. Covered California and the Department of Health Care Services have working hard to educate all of the enrollers and agents to understand the process of the Automatic Plan Selection. If you don’t understand something that has been sent to you, call Covered California that will have a special customer service staff just for the Automatic Plan Selection process or a health insurance agent.


