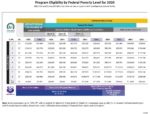
Covered California screens for Medi-Cal eligibility based on your monthly income, not annual income. Therefore, it is imperative, that when you are reporting a change to your income that the monthly income be accurate relative to published 138% of federal poverty level for adults and 266% for children.