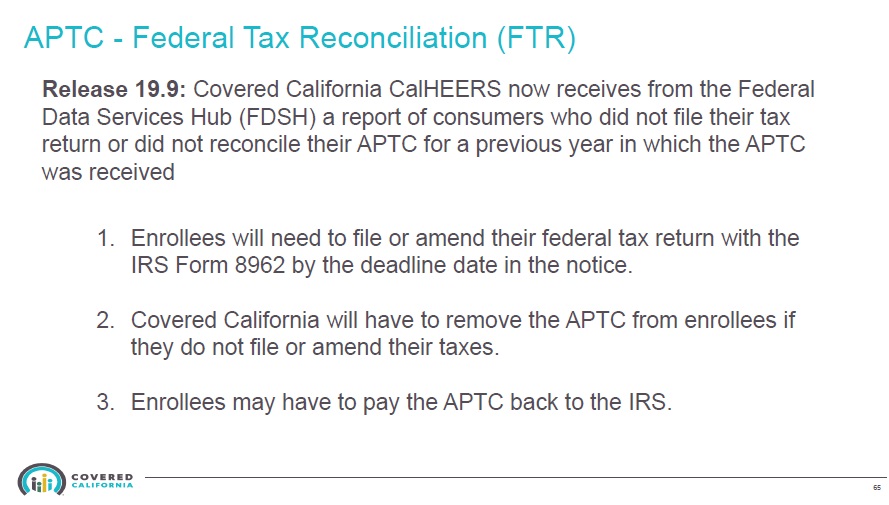
Covered California has updated their online application for renewing and new consumers to select a health plan for 2020. They have also integrated more communication with the Federal Data Service HUB to quickly check if household members have access to government sponsored health insurance such as Medicare and to determine if the tax payer in the household has filed their federal income tax returns reconciling their subsidies for 2018.
2020 Renewal Process
Consent for Verification
Consumers must update their consent for verification. If consent for verification terminated in 2019, and it has not been updated to at least 2020, the household will be renewed into the same plan, if available, but with no subsidies.
Medi-Cal Renewal
Covered California is offering a new feature to renew Medi-Cal coverage. Even though the household situation may have changed (more or fewer household members, change of income, change of immigration status, etc.), all of which can be updated on the Covered California account, the changes must also be communicated to the county Medi-Cal office. Verification documents can be uploaded into the Covered California system and reviewed by Medi-Cal case eligibility workers. But it is Medi-Cal at the county level that makes eligibility determinations so you must ensure they get the documents and know you have a change in the household.
Opt-In for Subsidies
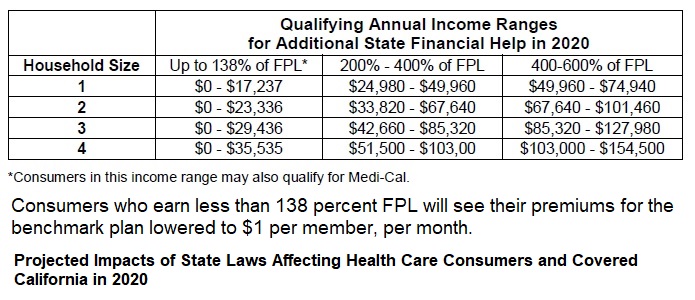
If a household entered Covered California and opted out of being considered for subsidies, during the renewal period, consumers can flip the switch on. This will trigger additional pages to be added to the application that must be filled out such as the income section. If you want to be considered for the new California Premium Subsidy for incomes between 400% and 600%, you will want to opt into the “Yes, I would like to see if I qualify for help from one of the available programs.”
The next steps of the renewal process will take the primary applicant to the different application sections to either confirm the existing information or make changes.
2020 System Renewal Mode
When the Covered California system is in the renewal mode, changes to your household will affect enrollment and subsidies for 2020. If you need to make changes for 2019, you will want to go through the Report A Change function on the home page. With that noted, the Open Enrollment period, Renewal period, coupled with current year changes has led to errors for the Covered California system in the past. Covered California has worked hard to correct those issues separating enrollments for 2019 from 2020. If you are in doubt about a change you are making, and which enrollment it might impacted (current or 2020) call your agent or Covered California.
Changes to Income
If you had previously used the Projected Annual Income edit feature to estimate your income different from the various income categories (wages, self-employment, capital gains, interest, dividends, Social Security, etc.), making changes to the specific categories will not change the final income estimate. That is because it is overridden by the Projected Annual Income field. You will need to navigate to that field and update it. Always check that your Monthly AND Annual estimated income amounts concur with one another.
Automatic Renewal
The Covered California system will automatically renew consumers into their same 2019 plans for 2020 based on existing household information. At any time before December 15, 2019, a consumer can make changes to the household data and select a different plan to begin January 1, 2020. However, if a current 2019 plan is not offered in the consumer’s region, they must select a new plan by December 15th. Applications that will not be automatically renewed are MAGI Medi-Cal only cases, and applications that were terminated before October 12, 2019.
Report A Change
If the 2020 renewal process has been completed, you can still Report A Change to the application for 2020. When you select the Report A Change button on the homepage, it will ask if you want to report a change for 2019 or 2020.
Theoretically, if you report a change for 2019, such as deleting or adding a household member, income change, or pregnancy, that information should flow to the 2020 application even if you have been automatically renewed. The Report a Change guidance document does not touch on that scenario. You will need to check your 2020 enrollment to make sure the 2019 changes flowed into the 2020 application. This means that you may have to select a plan for the new household member and review income and subsidy amounts.
Households are under no obligation to report a pregnancy. When you report a pregnancy, the system will screen for Medi-Cal eligibility with the increased household size with the number of babies expected to be born.
Through the Report A Change function, a consumer can change their application type from “No, subsidy consideration” to “Yes, I want to be considered for subsidy assistance.” Consumers who are already being considered for the federal and state subsidies cannot switch to “No, subsidy consideration.”
Household Eligibility Results Summary
It is important to review the eligibility results for each household member after the application has been submitted and the eligibility results page is available. You can view why Covered California made certain eligibility determinations with the view button.
If a pregnant person is eligible for more than one program, a Switch button will be displayed in the Summary View section to make a change. Consumers can also view documents Covered California has requested to verify certain household elements such as income or citizenship.
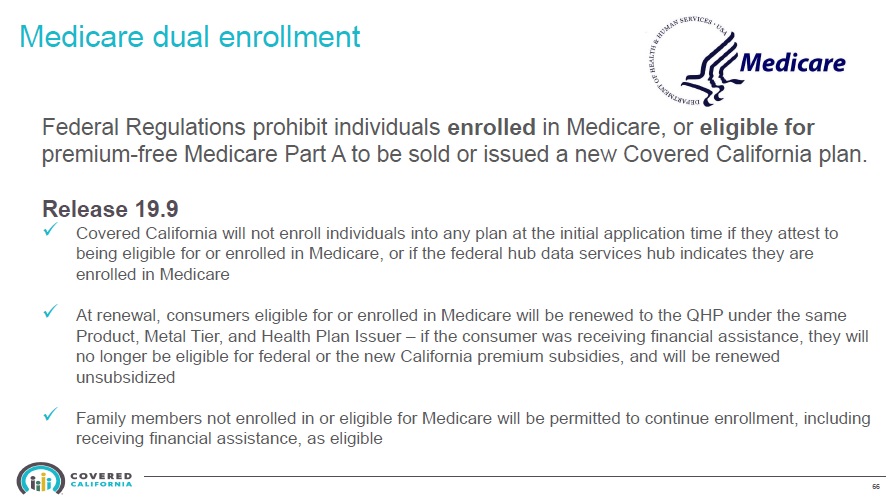
The Evolution of the Covered California Application
The CalHEERS (California Healthcare Eligibility, Enrollment, and Retention System) online application for Covered California has been completely remodeled from its origins in 2014. While many of the changes are cosmetic in order to help consumers navigate the complex enrollment process, Covered California has also been slowly adding other elements to bring it into compliance with the Affordable Care Act regulations. For instance, in previous years, it was all too easy for a consumer who was Medicare eligible to keep their Covered California subsidy because it was less expensive than enrolling in Medicare. A couple of years ago Covered California added a question whether any of the household members were in Medicare Part A. If you have Part A of Original Medicare, you were ineligible for the ACA premium tax credits through Covered California.
Covered California has now established a link with the Federal Data Service Hub to screen consumers to see if they are enrolled in Medicare Part A. If the system determines they are, they are ineligible for the subsidy tax credit.
On the latest iteration of the CalHEERS program, they have further refined the vetting process of household members to deny certain people to enroll on the family plan. This might occur if the household member is not eligible for subsidies or has qualified for an American Indian – Alaska Native health plan. This is not necessarily a bad thing. If you have ineligible household members getting subsidies, then the 1095A, the form that reports the subsidy amounts to the IRS, needs to be corrected before filing an income tax return. Correcting the 1095A can be time consuming and complicated.
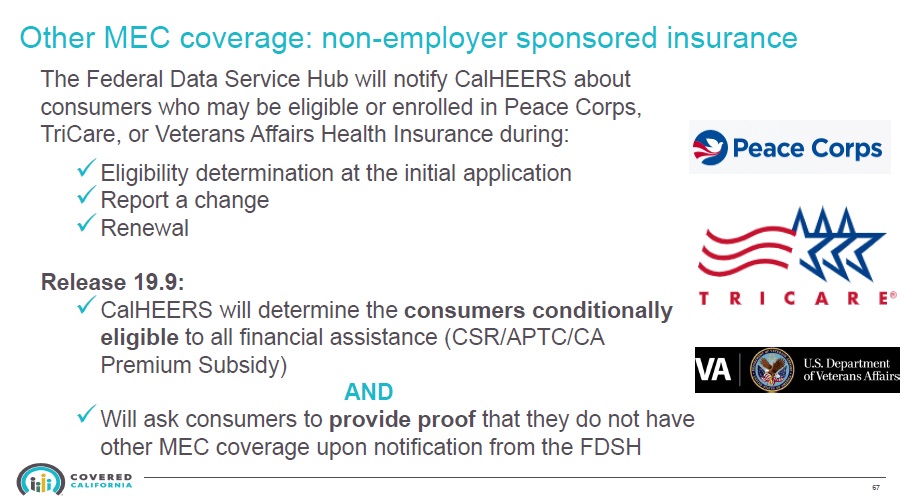
Additionally, a person does not qualify for the subsidies if they have government sponsored health insurance from the Peace Corp, TriCare, or Veterans Affairs. The Covered California system with reach out to the Federal Data Service HUB to check enrollment. If the search comes back positive, the person will be conditionally enrolled into Covered California. They will have a window of time to verify that they do not, in fact, have that government health plan.
Ineligible for Medi-Cal
The new California Premium Subsidy program will be extended to lawful permanent residents who are ineligible for Medi-Cal and have incomes under 138% of the federal poverty level.
State Subsidy and Mandate Fact Sheet
California will be the first state in the nation to provide state subsidies to many middle-income consumers who had previously not qualified for financial help because they exceeded federal income requirements.
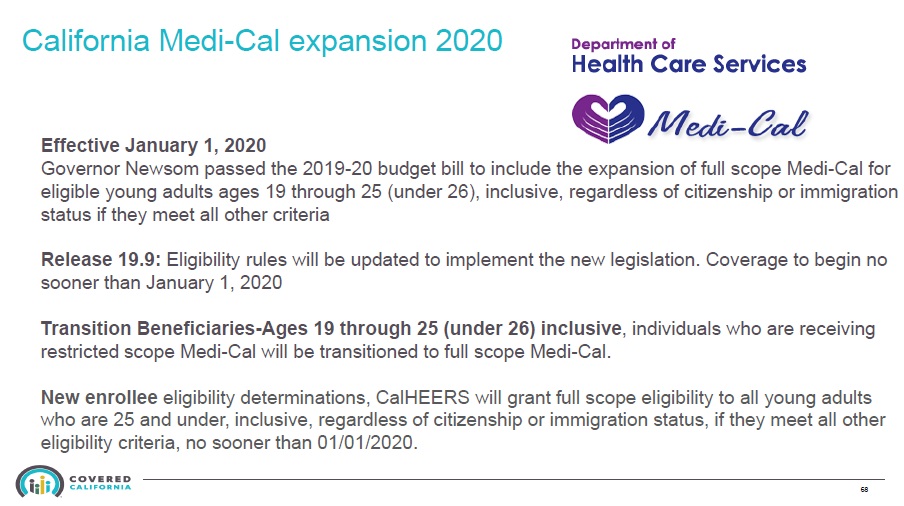
Medi-Cal
In 2020, young adults who did not have the proper citizenship or immigration status to enroll in Medi-Cal will be able to obtain Full Scope Medi-Cal. Young adults in this category, ages 19 through 25, will be able to apply for the Medi-Cal coverage that will be effective January 1, 2020 through Covered California.
Podcast
2020 CC IFP
- 1095A_FTB3895
- Apply_Change_SEP_1095A
- Cal Health Ins Penalty
- Cal Premium Subsidy
- Dental Adult Family
- Renew Coverage
- 2020 California Health Plan Basics Slides
- Conditional Eligibility Guidance Verification Documents
- Consent for Verifcation Guide
- Covid_19 Covered California Special Enrollment Period
- How to Delegate an Agent in Covered California
- Medicare_Attestation_Form
- New_Special_Enrollment_State_Subsidy_and_Individual_Mandate_QLE_Quick_Guide_Final
- Notification Of Deceased By An Enrolled Member
- Revised Covered California Medi-Cal Income Table for 2020
- Special_Enrollment_Period_for_State_Subsidy_or_Penalty_Fact_Sheet
- X_2020 Subsidy Eligibility Income Chart Covered California 9_2019