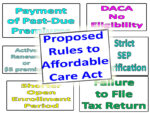
The main takeaway is that the calculations for the ACA health insurance income estimates are separate from determining the tax on Social Security benefits. Specifically, all the Social Security income is included on the Covered California application as income, but only ½ is used for the combined income calculation of Social Security income taxes.