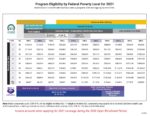
The confusion lies in the statement that the consumer is not eligible for the California Premium Subsidy. The California Premium Subsidy program is completely separate from the federal Premium Tax Credit subsidy. You can be eligible for the federal subsidy but not the State subsidy. If your income is over 400 percent of the federal poverty level, you are not eligible for the federal Premium Tax Credit subsidy, but you may be eligible for the State subsidy.