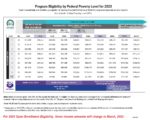
Many people do not update their income every year. While the income stays static, the threshold for Medi-Cal creeps up. The 2022 federal poverty levels are being applied for the 2023 Covered California subsidy and Medi-Cal eligibility. Many families are being caught by surprise that their current income is too low to maintain subsidies for their children.